Celiac disease is a serious genetic autoimmune disorder where the ingestion of gluten leads to damage in the small intestine. Therefore, people with celiac disease must eat a gluten-free diet. The disease affects 1 in 100 people worldwide, and one in 133 people in the United States. Two and one-half million Americans are undiagnosed and are at risk for long-term health complications.
Gluten, the culprit, is a family of dietary proteins found in wheat, barley, rye, oat, and other grains. It is the protein that makes dough elastic and gives bread its chewy texture. It is naturally poorly digested, and therefore more likely to engage the immune system than other proteins, even in people without celiac disease.
In people with celiac disease, it damages the intestinal villi, which are very small finger-like projections found along the wall of the small intestine. When the villi are injured, the small intestine can’t properly absorb nutrients from food. So, again, people with celiac disease must avoid foods that contain gluten. Sometimes, they may feel isolated, as they must eat differently than others.
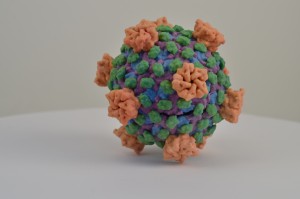
REOVIRUS. Image credit: NIAID, NIH, CC BY 2.0
But guess what? There is a new trend in college dining halls. They’re offering tastier gluten-free foods to attract students without food restrictions so allergy sufferers won’t feel isolated. The following is from The New York Times: “Out with pizza, in with poke bowls. That’s the new culinary strategy at Kent State and Cornell University, which this school year rolled out the first certified gluten-free dining halls. An estimated 5 to 10 percent of college students have celiac disease or other gluten-related disorders, according to Dr. Alessio Fasano, director of the Center for Celiac Research and Treatment in Boston. For them, avoiding gluten—wheat, rye, barley and cross-contaminated oats—isn’t a fad diet but a medical necessity. Even a bread crumb in the communal cream cheese could wreak gastrointestinal havoc, causing symptoms that lead to missed classes and more. A 2016 survey by the New England Celiac Organization concluded that “college students with celiac disease and gluten sensitivity face overwhelming complications in their social and academic lives.”
And…. we have not only a new trend in college dining halls, but also new insight in what actually causes celiac disease. A new study (Reovirus infection triggers inflammatory responses to dietary antigens and development of celiac disease), published last week (April 7, 2017) in the journal Science, shows that Infection with reovirus, a common but otherwise harmless virus, can trigger the immune system to react to gluten, leading to the development of celiac disease. How? Usually, a regulatory immune response blocks inflammation to dietary antigens. However, a reovirus infection at sites where dietary gluten is present results in the induction of danger signals that confuse the immune system and lead it to develop an aggressive inflammatory immune response against gluten—it is this aggressive inflammatory response that may induce celiac disease.
For the study, which was carried out in a mouse model, researchers used two different closely related but genetically different reovirus strains. They showed that genetic differences between viruses can change how they interact with the immune system. Both reovirus strains induced protective immunity and did not cause overt disease. However, one of the reovirus strains triggered an inflammatory immune response and the loss of oral tolerance to gluten, whereas the other strain did not.
Bana Jabri, the study senior author, said in a press release: “This study clearly shows that a virus that is not clinically symptomatic can still do bad things to the immune system and set the stage for an autoimmune disorder, and for celiac disease in particular. However, the specific virus and its genes, the interaction between the microbe and the host, and the health status of the host are all going to matter as well.”
The study also found that celiac disease patients produces much higher levels of antibodies against reoviruses than those without the disease. The celiac patients who had high levels of reovirus antibodies also had much higher levels of IRF1 gene expression, a transcriptional regulator that plays a key role in the loss of oral tolerance to gluten. This suggests that infection with a reovirus can leave a permanent mark on the immune system, a mark that sets the stage for a later autoimmune response to gluten.
in the United States, babies are usually weaned from breastfeeding and given their first solid foods—often containing gluten—around six months of age. Children with immature immune systems are more susceptible to viral infections at this stage, and for those genetically predisposed, the combination of an intestinal reovirus infection with the first exposure to gluten could create the right conditions for developing celiac disease.
“During the first year of life, the immune system is still maturing, so for a child with a particular genetic background, getting a particular virus at that time can leave a kind of scar that then has long term consequences,” Jabri said. “That’s why we believe that once we have more studies, we may want to think about whether children at high risk of developing celiac disease should be vaccinated.”



I think this is a groundbreaking discovery as so many people are affected by celiac disease. Hopefully, this will help foster further research not only to prevent celiac disease but also to possibly cure those who already have it. After doing some research, I found that reoviruses are oncolytic and are being looked at as potential treatments for cancer. In a study done by Kim et al., it was found that an attenuated reovirus targeted cancer cells in severely immunodeficient mice without killing healthy stem cells. The attenuated reovirus also exhibited reduced toxicity compared to a wild-type reovirus . The study also implies that attenuated reoviruses could be used to treat cancer in pregnant women (1). With the recent connection of reoviruses to celiac disease, I cannot help but wonder whether this will influence their potential use for treating cancer. Could reovirus cancer treatments cause an individual to develop celiac disease? If children infected with reovirus are at a higher risk of celiac disease, are reoviruses really safe to use for cancer treatment in pregnant women?
1. https://www.ncbi.nlm.nih.gov/pubmed/21179029
Megan,
I find all the points you discuss fascinating – thanks for sharing. I didn’t know that reovirus was being used as a treatment for cancer. Going off on your comment, I decided to investigate the specific cancers that use reovirus-based therapy. I found out that reovirus can be employed for the treatment of pancreatic cancer, and is more effective if used in combination with other drugs. (1) Reolysin (the drug name that uses reovirus) works by inducing stress in the endoplasmic reticulum, which eventually leads to apoptosis. Amazingly, Reolysin can selectively attack the cancerous cells due to reovirus’ ability to differentiate cells that express mutations in activated Ras signaling, specifically KRas. These mutations help facilitate viral uncoating and production of viral progeny in the cell. (2) I do share your concerns though about the potential side effects of using reovirus as a treatment – this should be thoroughly studied as the treatment looks quite promising.
1. https://www.ncbi.nlm.nih.gov/pubmed/23868061
2. https://www.ncbi.nlm.nih.gov/pubmed/25019061
Over the past couple of years, scientists are starting the discover the importance of gut microbial and its effects on food digestion and the immune system. In the case of Celiac Disease, a virus or maybe a bacterial infection can affect the intestinal tract leading to developing celiac disease. But what about other autoimmune diseases that deal with food absorption? According to a new study (1) gut, microbial metabolites protect against type 1 diabetes. In this study, they took mice that had type 1 diabetes and fed them a diet that would increase the amounts of acetate and butyrate released by gut microbial. It turns out that if your gut microbial produce increase levels of acetate it decreases the frequency of autoreactive T cells in lymphoid tissues. Acetate effects the B cell preventing them from activating more autoreactive T cells. Increased levels of butyrate increased the number and function of regulatory T cells. It appears that dietary changes for people with T cell-dependent autoimmune diseases may be an effective natural way of treatment. Another study (2) suggested that there might be a connection between an accumulation of autoreactive T cells in the gut-associated lymphatic tissue and other autoimmune diseases such as multiple sclerosis. I think we often overlook our diet and how it affects our overall health and not just our waistline. These emerging studies could also lead to new noninvasive ways of treatment.
1. https://www.ncbi.nlm.nih.gov/pubmed/28346408
2. https://www.ncbi.nlm.nih.gov/pubmed/27856664
Shannon, it is so interesting that autoreactive T cells could do so much damage and contribute do a disease that is widely accepted as a genetic disorder. This post made me want to look up what else autoreactive T cells could do in the human body and I found that they are also a large part of development of Rheumatoid Arthritis (1). The autoreactive T cells actually reduce glycolysis and cause the CD4+T cells to hyperproliferate and attain the inflammatory symptoms we see as symptoms in Rheumatoid Arthritis. This made me wonder what dietary changes could these patients make to reduce their levels of autoreactive T cells? According to a new study (2), by taking a fish oil supplement can reduce the number of autoreactive T cells all together. They also showed in this study that the fish oil also promoted an increase in CD8+ T cells in mice. More supporting evidence was found in another study (3) that showed that fasting in regular intervals also decreases autoreactive T cells that contribute to multiple sclerosis symptoms. Seeing how diet can influence all of these major diseases is eye opening and definitely needs to be explored as alternative or combination treatments for patients.
1. https://www-ncbi-nlm-nih-gov.ezproxy.gsu.edu/pubmed/28360422
2. https://www.ncbi.nlm.nih.gov/pubmed/11321127
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899145/
Researchers are connecting the dots more and more everyday between autoimmune diseases and bacterial infections causing them. In a recent study, a connection was made between gut mycobacteria imbalance and the development of Chron’s disease as well as ulcerative colitis (1). There is a very particular balance of bacteria that are good for us and help digest our foods for us throughout our digestive tract, but when this balance is lost, some of the bacteria can grow exponentially, causing havoc in the gastrointestinal system. The bacteria is kept in check by our bodies by controlling the pH and temperature along the GI tube, when these checks are overridden the bacteria are allowed to have a field day and grow without being controlled by the host body. One study that was found recently, focuses on what happens to your gut microbiome when you starve the body of carbohydrates as in a ketogenic diet (2). As you starve your body from carbohydrates to try and lose weight the Bacteriodes that call your gut home and whose sole purpose is to digest carbs begin to die off. This pruning of the gut microbiota allows for more invasive species to overgrow and populate areas of the GI tract that they usually are not found in. This also promotes the growth of very harmful strains of bacteria to grow that are usually kept in check by the growth of the Bacteriodes, such as Clostridium difficule (2). The research on this topic is now pointing toward the overgrowth of some bacteria getting through the gut walls and into the abdominal cavity to elicit an immune response. After a prolonged period of bacteria entering the gut, the body starts to see the intestines as foreign cells, and it immune system shifts its focus to fighting off the ‘invader,’ that is actually the body’s own cells. This is what is supposedly causing the autoimmune diseases such as Chron’s.
1.https://www.ncbi.nlm.nih.gov/pubmed/21988043
2.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608238/
Emily,
With research coming out on how viruses and bacteria can cause autoimmune diseases it makes you wonder how strong a role genetics play. It seems like gut flora is the missing link for a lot of diseases. In “Does the Gut Microbiota Influence Immunity and Inflammation in Multiple Sclerosis Pathophysiology?” their aim was to determine if gut microflora plays a role in developing MS (1). While it is unclear how exactly gut microflora contributes to the development of MS, there is a relationship. As you mentioned earlier a stable gut flora protects against inflammation. In another study, it was noted how there are gut microbiota-host interactions that play a role in the development of cardiovascular diseases (2). Again, the pathophysiology is unclear but with immerging studies I imagine the relationship will soon be discovered. I think more research so go into the gut-immunity-brain axis.
(1) https://www.ncbi.nlm.nih.gov/pubmed/28316999
(2) https://www.ncbi.nlm.nih.gov/pubmed/28360349
This article was very interesting to me as it pertains to gluten and how reovirus plays a part in celiac disease. Many people suffer with gluten and have to take great measures to get by day by day. One thing I found interesting was the idea how reovirus, usually considered an inoffensive virus, can “trick” the immune system to believe that gluten is harmful and causes the immune system to have a belligerent response to gluten. This is dangerous not only to adults but the article also pointed out that it can be critical to children and infants. Studies have been done to test rotavirus vaccinations in children with celiac disease as well as type 1 diabetes (1). According to Outi, their studies suggest that this vaccination can be beneficial for children who have a high chance of contracting celiac disease or type 1 diabetes. This research is just the tip of the iceberg in learning more on the relationship of rotavirus and celiac disease.
Reference:
1. Rotavirus Vaccination and the Risk of Celiac Disease or Type 1 Diabetes in Finnish Children at Early Life. https://www.ncbi.nlm.nih.gov/pubmed/28399059
Offering tastier gluten free foods should be a major matter in the upcoming years. Not only gluten free diet reduces the tragedy of celiac disease; but it also minimizes the symptoms associated with schizophrenia. A study that was published in April 2017 showed that schizophrenic patients who follow a gluten free diet suffer way less than those who have gluten included in their diet (1). Gluten could be associated with more diseases and some more studies on gluten effects on the human body should be done. Therefore, having tastier gluten free foods available in schools, hotels, hospitals, restaurants, ..etc. should be a major concern within the next years.
1) https://www.ncbi.nlm.nih.gov/pubmed/28393621
Ajudeh1,
Your comment on how gluten-free options can reduce symptoms of schizophrenia is interesting. I do not know much about schizophrenia but I know people with this disorder suffer with the symptoms associated as well as the community surrounding them. I believe having a gluten-free diet benefits these individuals in more ways than one. I found an article stating how athletes who adhere to a gluten-free diet had better success in their goals as well as their body systems (1). Little is known on this study but it’s interesting how gluten-free diets can be beneficial for anyone.
Reference:
1. https://www.ncbi.nlm.nih.gov/pubmed/27399823
Coeliac disease is a serious ailment affecting more and more children every year. Because of the rapid increase in coeliac disease diagnosis, it is important to diagnose exactly what type of gluten-related disease a person has. Depending on the severity of the coeliac disease, doctors can determine a patient’s ideal diet to decrease the negative effects of the disease and better the overall lifestyle of the patient. In a study done recently, it was reported that anti-glutaminase antibodies are specific for the diagnosis of coeliac disease and in determining specific symptoms [1]. There are three specific gluten-related disorders: coeliac disease, wheat allergy, and noncoeliac gluten sensitivity. However, further research must be conducted to better understand noncoeliac gluten sensitivity as not much is known about this disease. It is important to conduct research on, not only coeliac disease but also, the other kinds of gluten-related ailments. These are important especially in relation to the health of young children. It is detrimental to the already fragile immune system of a child to develop coeliac disease. Like this blog post mentioned, this disease can affect all aspects of someone’s life and, as an aspiring pediatrician, I would like to see more emphasis on discovering how to aid children in preventing coeliac disease.
1. https://www.ncbi.nlm.nih.gov/pubmed/26100369
I had heard of celiac disease before but I was unaware that there were other gluten related disorders. After reading your post, I agree that there needs to be more research into these disorders as well. In a study by Unde et al., they attempted to identify markers for systemic immune activation in wheat sensitive individuals who did not have celiac disease. They determined that these individuals had higher levels of CD14 and LPS-binding protein in their serum. They noted that there was systemic immune activation because of antibody reactivity to bacterial LPS and flagellin. They also found levels of fatty acid-binding protein 2 which indicated damage to the intestinal epithelium (1). I think more research like this will bring other gluten sensitive disorders to light. It may also help us determine more distinctions between celiac disease and other gluten related sensitivity disorders.
https://www.ncbi.nlm.nih.gov/pubmed/27459152
I have always been interested in studying Celiac disease. I always wanted to learn why and how it affects so many people. I also would not mind trying to find a cure for the disease.
I remember I had a friend during my first year of college who was very strict about avoiding foods containing any gluten at all. At first, I thought that she was avoiding foods containing gluten due to some sort of a diet fad or something of that nature. However, I later discovered that she was allergic to gluten and had suffered complications earlier in her life due to damage in her small intestine. I remember some of our mutual friends would be annoyed whenever we would want to eat certain items but she would always have us change our plans to eat something that was gluten free instead. I can thus relate to the article in that people who are allergic to gluten or have Celiac disease oftentimes feel isolated with limited options and with friends who are not interested in sharing gluten free meals with them. I think there should be a bigger push across college campuses to include more gluten free options that are enjoyable for both those who are unable to eat gluten and for their friends as well.
I also found it fascinating that the Reovirus is involved with Celiac disease induction. Another study has also described an association between Celiac disease and chronic Hepatitis C caused by the HCV virus (1). It will be interesting to see what other pathogens contribute to Celiac disease and what preventative measures (such as vaccines) can be employed to prevent the development of Celiac disease in the first place.
1. https://www.ncbi.nlm.nih.gov/pubmed/27458507
Joshua Thomas,
I agree with your comment; the school should have more gluten free options for some people.I didn’t know much about gluten when I was growing up. I used to hear commercials talking about gluten-free products, and I thought it was just that product that had gluten. It turns out most of the stuff we eat have gluten. It must be a real pain to have that allergic reaction. However new studies have alternative ways for Celiac disease treatment without avoiding gluten products. In a study done by Marino and his colleagues shows that modification of gliadin peptides inhibits their ability to induce an immune system response. This is done by using microbial transglutaminase for the change of the gliadin peptide. This is a good alternative, but there are some side effects we know about and some we don’t. Since this is relatively new, we don’t know long-term side effects. Eating gluten free products is the best choice.
https://www.ncbi.nlm.nih.gov/pubmed/28343108
I find this article to be very informative since I was not so familiar with celiac disease and how exactly it effects the human body. I have noticed a change in the food diets of our country that now normalizes gluten-free products. Just as the article mentioned, I inferred that gluten was another fad diet that was avoided by the general public to lose weight or become healthier. Though this study initially mentions it is mainly the presence of gluten itself that damages that lining of the small intestine, multiple studies have also included reovirus as being the cause for the immune confusion and eventual self-attacking episodes. The article Celiac Disease: Reovirus, Inflammatory Response, and Dietary Antigens agrees with the correlation between the reovirus and celiac disease and wanted to take studies further with a vaccine. Since there has been a vaccine made for celiac, their job was to test out the vaccine and see if there may have been an increased risk of actually developing the disease in children. However, after testing out a large amount of subjects throughout a five-year study, they did not see an increase in children with the vaccination than children without the vaccine. Though more trials may still need to be done as for the effectiveness of the vaccine against the virus, a negative correlation is currently not found.
1. https://www.ncbi.nlm.nih.gov/pubmed/28399059
I, too, was not aware of celiac disease and how many people it affects. I’m glad i got a chance to read about it, it opened my eye to something I’ve been so unaware about for so long. It’s refreshing ti know our country is making more and more gluten-free diets as this condition affects more and more people each year. It’s never easy living with an autoimmune disease, and it is very informative to know more research are being done about the causes and the possible correlation this disease has with the reovirus virus. Even possibly a vaccine for the disease.
1. https://www.ncbi.nlm.nih.gov/pubmed/28386004
This post talk about how reovirus can trigger celiac disease by inducing the immune system to react to gluten. They also found out that there is higher level of reovirus antibody present in the patient with celiac disease compare with those who without the disease. Not all reovirus strains can trigger the autoimmune reaction. During their study, they found out that the ability of the strain to trigger the inflammatory immune response is depending on their genes since reovirus with different genes interact with the immune system differently. Autoimmune disease, especially inflammation of the digestive track, has been close linked to the viral or bacterial infection by many researches. Under normal condition, the intestinal mucosa is protected by the tight junction which limit the passage of the foreign antigen. Many of the research shows that certain kinds of virus or bacteria can modulate the intercellular tight junction and therefore, the intestinal mucosa permeability is increase. When the permeability is increase some foreign antigen such as gluten and other diary antigen can pass through the gut mucosal barrier and cause inflammation. The mechanism that those antigens trigger autoimmune reaction is called “molecular mimicry” which microbial antigens are postulated to resemble self-antigen (1). I think that the reovirus play an important role in the “molecular mimicry “mechanism of gluten. Once the autoimmune reaction is activated, it becomes independent of continue exposure to the environmental trigger and therefore self-perpetuating and irreversible (2) which means the autoimmune reaction cannot be shuttled off although the triggered antigen is being removed. Many of the inflammation bowel disease such as Crohn’s disease and ulcerative colitis is triggered by the incontrollable immune system. Many people may ask why gluten consumption is very susceptible in triggering autoimmune reaction? The reason for this is that gluten is made up of gliadin and glutenins which contains many toxic epitopes that can exerting cytotoxic and other gut permeating activities. Celiac disease also has close genetic association with HLA genes which is a highly specific humoral autoimmune response against tissue transglutaminase auto-antigen (2). The present of gluten in the GI track also lead to upregulation of the zonulin which is the only physiologic modulator of intercellular tight junctions described so far that is involved in trafficking of macromolecules and, therefore, in tolerance/immune response balance (2) and people with acute celiac disease have higher level of zonulin. Therefore, gluten is very susceptible in triggering the autoimmune disease and I think that future study can be conducted to investigate the relationship between the reovirus infection and the zonulin pathway.
1. https://www.ncbi.nlm.nih.gov/pubmed/15286377
2. https://www.ncbi.nlm.nih.gov/pubmed/22109896
Celiac disease is one of many severe autoimmune diseases known to cause cancer cells. The fact that 2.5 million Americans are undiagnosed and risk complications due to long term exposure, indicates the urgency for intervention and development of vaccination. Human leucocyte antigen (HLA) is a cell surface protein receptor for MHC class II antigen presenting cells. Gluten proteins, in the small intestine mucosa of patients infected with reovirus, readily binds HLA antigen DQ (HLA-DQ2 or -DQ8) with high affinity and activates T cell specific for gluten proteins that cause destruction of intestinal vili (1). Addison’s disease, autoimmune thyroid diseases, and Type 1 diabetes are examples of endocrine disorders that exhibit genes for HLA autoimmune response. Therefore, gluten proteins in reovirus infected patient, will cause celiac disease and may induce other HLA-linked diseases that is detrimental to our health.
1. https://www-ncbi-nlm-nih-gov.ezproxy.gsu.edu/pubmed/25925917
Celiac disease is a severe genetic autoimmune disorder in which the gluten digestion leads to the small intestine being damaged. When people with is disease take in food with gluten, the body sees this as a foreign invader and sends a signal to the immune system, which attacks the small intestine. The only treatment available for people with this disease is a strict gluten-free diet. With more awareness being brought forth by this disease, it should also start the discussions about the many other autoimmune disorder relating to food or not. For example, pernicious anemia, the autoimmune condition in which the body absorption of B12 is flipped, resulting in a B12 deficiency (1). Of course, more studies can be done to get to the bottom line of why autoimmune exists in the first place. But in the case of celiac disease, it is an enormous progress that society is more aware and understanding of the importance of a gluten-free diet and making it more available.
1. https://www.ncbi.nlm.nih.gov/pubmed/28360040