A recent opinion article in the New York Times Sunday Review (Pregnant, Obese … and in Danger) highlights the dangers of obesity in pregnancy and childbirth. The article’s author, obstetrician and gynecologist Claire A. Putnam, states that: “Over two-thirds of adults and about one-third of children in America now are overweight or obese. An obese pregnant woman is more likely to have a very large baby, weighing roughly nine pounds or more. And babies of obese mothers are more likely to grow up to become overweight or obese themselves. Maternal obesity causes more immediate problems as well. Obese pregnant patients are more likely to have elevated blood pressure, gestational diabetes and babies with birth complications. They are more likely to need cesareans. And they are more likely to have serious complications from the surgery, such as infections, hernias or life-threatening bleeding.”
But what about babies born to obese mothers? In addition to birth complications, are there other consequences for these babies? Unfortunately, the answer is yes. Maternal obesity is linked to several adverse health effects in the offspring — and these effects may persist into adulthood. Babies born to obese mothers have increased lifelong risk of obesity, type-2 diabetes, high blood pressure, heart disease, asthma, and other disorders that involve the immune system. Indeed, results from a recent study show that changes in the immune system are already detectable at birth.
For the study, researchers analyzed umbilical cord blood samples of infants born to mothers grouped in lean, overweight and obese categories. These three categories were established on the basis of the body mass index (BMI) — the BMI is a measure of body fat, and is indicated with a number calculated from height and weight. A mother was considered overweight if her BMI was 25 to 29.9, and obese if her BMI was 30 or higher. The researchers found that pre-pregnancy maternal weight has a significant impact on the immune system of the neonate.
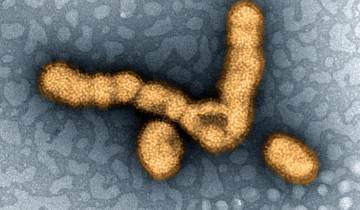
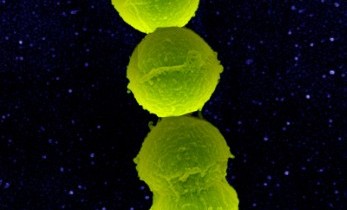
Ilhem Messaoudi, lead author of the study, said in a press release: “We found that very specific immune cells in circulation — monocytes and dendritic cells — isolated from babies born to moms with high BMI were unable to respond to bacterial antigens compared to babies born to lean moms. Such babies also showed a reduction in ‘CD4 T-cells.’ Both of these changes could result in compromised responses to infection and vaccination.”
The researchers also found that eosinophils — cells that play a role in allergic response and in the pathogenesis of asthma — were significantly reduced in the umbilical cord blood of babies born to obese mothers. One potential explanation for these observations is that these cells have already moved into the lungs, which could explain the increased incidence of asthma observed later in life in children born to obese mothers.
Messaoudi added that the immune system changes detected in babies of obese mothers could influence the response of these babies to vaccination and to asthma-inducing environmental antigens. He said: “As we know, in the first two years of life, children typically receive plenty of vaccines. The questions that arise are: Are the responses to vaccines in infants born to obese moms also impaired in the first two years of life? Should we change how often we vaccinate children born to obese moms? Should we change practices of how much and how often we vaccinate?” Messaoudi sees the study results as a launching point for further studies and a call to action.
During prenatal visits, doctors talk to pregnant mothers about smoking, recreational drug use, and alcohol. However, they should also talk about weight and weight management. In addition, as Claire A. Putnam states in her opinion article: “Above all, we need to end the taboo against talking frankly about obesity. Doctors need to be sensitive and nonjudgmental, and patients should not take offense, especially when their health, and their children’s health, is at stake.”



As an aspiring physician, this article fascinated me for many reasons. Firstly, the article screams out the importance of educating the public. I mean, it isn’t the first time we have all hear that obesity is some what of a silent killer. Not only is it detrimental to your cardiovascular system, but it causes strokes, depression, metabolic syndrome, and encourages other diseases like diabetes. Time, and time again, it has been shown that efforts to properly educate the public results in positive actions. But frankly, I think our scientific community isn’t done enough to change the public’s perspectives on this national crisis of obesity. Targeting obesity is no longer a New Years resolution, but as this article mentioned, it is now concerning the functionality of their overall health of the future generation. Therefore, it isn’t enough to release annual statistics on America’s obesity rate. We must find new methods to educate the public and assuage this endemic. Also, I did a little dig and found a report from the CDC, that stated that, in 2008, $147 billion dollars were spent in the United States on healthcare relating to obesity. I, by no means, undermine the complexity of obesity. I fully understand that the issue of obesity stems from demographic, financial, psychological, and social influences and, therefore, it can not be resolved with a one-size-fits-all solution. But at least a quarter of that $147 billion spent, could have been utilized in cancer research, for example, if more was done to alleviate the growing rate of obesity.
Science already proved that genetics play a major role in obesity .Genes can directly cause obesity in disorders such as Bardet-Biedl syndrome (which affect many part of the body causes hormonal imbalance, diabetes, vision impairment ,intellectual disability)and Prader-Willi syndrome( which causes weak muscles,poor growth, unstable appetite , hyperphagia). However genes do not always predict future health. Eating healthy diet and having enough excercise can overcome the issue of hereditary weigh gain issues.Apart from all these Obesity can affect fertility by causing hormonal imbalances and problems with ovulation, particularly for obese women having their first baby. Obesity is associated with poly-cystic ovary syndrome (PCOS), a common cause of infertility.Obese mothers have high risk of losing their baby due to miscarriage .All these issues and many more more was already known to the public or should be known to the public.The recent study is an additional threat to the obese population
While this is certainly an interesting study, and certainly an important point for medicine and science to work together on, I don’t find the results all that surprising. A mother’s health and health related choices having a direct effect on a fetus? It’s already well accepted that alcohol and tobacco can impact the wellbeing of fetal health. So to me, living in conditions considered medically to be unhealthy having a role in fetal development seems like a natural part of maternal health being impacted onto child.
What I find myself more curious about, and what I think could be a far more interesting link, would be “can the health and obesity of the father have a role on the health of the child?” It also probably comes as no surprise that one study found that obesity indeed can impact pregnancy rates. The study found that sperm from obese males weren’t very effective at actually penetrating the uterus. What was surprising, however, was that successful pregnancies from obese mice actually resulted in smaller than average fetuses. Further, it’s suggested that children born of these conditions have increased risk of developing type 2 diabetes and cardiovascular disease later in life. So as it turns out, obesity in the father may be just as influential in fetal development as maternal obesity!
Citation: Binder NK, Hannan NJ, Gardner DK (2012) Paternal Diet-Induced Obesity Retards Early Mouse Embryo Development, Mitochondrial Activity and Pregnancy Health. PLoS ONE 7(12): e52304. doi:10.1371/journal.pone.0052304
I really liked your comment, mostly because I didn’t even consider paternal obesity to have much effect considering how much of the development comes from the mother. I found it so interesting I went and did some more digging to find out what other effects paternal obesity may have on a fetus. There is an interesting study that was done in May 2015 that supports your point of an increased risk of type 2 diabetes. The study by Nicole O. McPherson et. al. found that female children have impaired insulin sensitivity when the father is obese. The most interesting part of this study is they subjected obese male mice to 8 weeks of exercise prior to conception and found restored insulin sensitivity. If this is relevant to humans it could be a great way to prevent diabetes caused by paternal obesity.
Initially, I found this statement to be a little hard to believe. The dietary habits of an obese mother can obviously affect the fetus. A pregnant patient with poor diet provides the fetus with high levels of glucose and fat that could, in fact, cause fetuses to be born overweight. Contrastingly though, for the father to be involved, obesity would now have to cause genomic mutations or some sort of genomic influence on the progeny’s diet. But apparently, genetic experts from Mount Sinai discovered, in 2007, “that individuals who carry two copies of a common variant of the FTO gene weigh on average 3 kg more than those who do not carry any copies.The genetic variant seems to predispose people to consume greater quantities of food.” So I agree, the father could be quite influential.
Willyard, C. (2014). Heritability: The family roots of obesity. Nature, 508(7496), S58-S60. doi:10.1038/508S58a
@Quentin Dolly it shouldn’t be too hard to believe that the father would also play a part in affecting the health of the fetus apart from just their genetic code, an example would be the case of that Shane stated with sperm not being able to penetrate the uterus. Another example would be epigenetics, modification of gene expression, an how alterations can even be done germ cells and carry to their progeny. A study done in 2013, though possessing a small sample size, found that obese father were likely to have hypomethalation of a growth factor gene, those genes would not be normally expressing, passed that hypomethalated gene to their offspring. So yeah, it is not a matter of just the weight of the mother affecting the baby, but the weight of the father also playing a role in the matter.
citation: Soubry, A., Schildkraut, J. M., Murtha, A., Wang, F., Huang, Z., Bernal, A., … & Hoyo, C. (2013). Paternal obesity is associated with IGF2 hypomethylation in newborns: results from a Newborn Epigenetics Study (NEST) cohort. BMC medicine, 11(1), 1.
I appreciate the studies that you both shared. But looking at the question Quentin posed regarding the effect of obesity on the genome, I’m curious to know more about the precise mechanism myself. The article I provided earlier referenced several impacts such as physically altering the size of the sperm, sperm fertilization efficiency, the size of the fetus, and some interesting alterations to blastocysts. For instance, it mentions that in vitro blastocysts derived from these sperm “showed reduced outgrowth on fibronectin” and that blastocyst allocation of cells going to the inner cell mass is reduced. They do speculate that alteration of gene imprinting could potentially cause changes to how blastocysts allocate cells to the ICM. Looking at the study C. Fischer provided, simple exercise for 2 months prior to conception was enough to restore insulin sensitivity in offspring. Based on that, it seems logical that genomic changes are not what’s impacting the insulin sensitivities in offspring. The article does go on to tie phenotype differences to microRNAs, which, while not genomic alterations themselves, do play a significant role in genomic expression. So that’s two separate studies both suggesting the role obesity plays is more in the field of epigenetics, as opposed to alteration of genome itself.
I already knew that if mother is obese, it can have bad effects on fetus but paternal obesity also affect fetus was something new to me. I was interested in seeing what other effects paternal obesity can have on fetus besides what my colleagues have mentioned above. I came across very interesting study that says paternal obesity could be a greater risk factor than maternal obesity. The researchers found that maternal obesity had a little association with the development of autism in the child. However, they found a doubled risk for development of autism and Asperger’s syndrome in the child if the father was obese, compared with a normal weight father. This study shows that till now we had too much focus on the mother and too little on the father. This probably reflects the fact that we have given greater focus to conditions in pregnancy, such as the growth environment for the fetus in the womb than both environmental and genetic factors before conception.
Based on the paper results, there may be a genetic link between obesity in the father and the development of autism in the child. Genetic mutation may play a role in the development of both extreme obesity and autism. Another explanation may lie in epigenetics. Epigenetic changes do not mean that the gene is altered, but that the gene is activated or inactivated as a result of environmental conditions. Switching a gene on or off at the wrong time and place can lead to adverse consequences for the individual and the genetic changes can be passed on to the next generation.
I feel that how epigenetic changes in germ cells are affected by obesity and environmental conditions can be a potential area of research.
Citation: Suren P, et al. Parental obesity and risk of autism spectrum disorder. Pediatrics, 2014
Ishita, when I first read the sentence regarding a study stating “paternal obesity could be a greater risk factor than maternal obesity”, I thought that sounded a bit too extreme. Initially, the paternal genome having an effect on offspring was surprising enough, however, looking more into it myself that link may be far more influential than I initially assumed, as your study suggests. One study I came across examined the ancestral role a paternal genome has by following multiple subsequent generations of mice. Specifically, they were curious if these epigenetically inherited traits could actually persist for multiple generations, something I would have assume wouldn’t be possible outside of genome alteration itself. According to their results, the answer to this question is a definitive yes. They went on to propose potential places within sperm, specifically with regard to DNA packaging, that are likely to be influenced by epigenetics and play a role later in embryo development.
With all that said, while the effects of the paternal line on embryonic development are interesting, I wouldn’t want to discount the essential role the mother clearly plays. I did come across a second study performing a very similar study, but studying the role of the maternal line over multiple generations, specifically observing the following three generations after feeding a mouse a high fat, high sugar diet. They determined persistent insulin issues were associated with mitochondrial dysfunction, a phenotype that could be passed down to the second and third generations in the maternal line.
All that to say, clearly the obesity epidemic in the country is far more concerning to me now knowing that it has the potential to be a much longer term issue than what I had originally assumed.
Citation: Yazbek SN, Spiezio SH, Nadeau JH, Buchner DA. Ancestral paternal genotype controls body weight and food intake for multiple generations. Human Molecular Genetics. 2010;19(21):4134-4144. doi:10.1093/hmg/ddq332.
Citation: Saben JL, Boudoures AL, Asghar Z, et al. Maternal Metabolic Syndrome Programs Mitochondrial Dysfunction via Germline Changes across Three Generations. Cell Reports. 2016;16(1):1-8. doi:10.1016/j.celrep.2016.05.065.
Epigenetics is ridiculously fascinating to me; I almost wonder if ten years from now I’ll be teaching a somewhat nuanced take on Lamarck instead of the ‘he was completely wrong’ take I grew up with. That paternal obesity could have an impact is amazing. I knew there are likely paternal age effects on offspring (Ramamsamy, Chiba, Butler, & Lamb, 2015), particularly in regards to potential correlation with schizophrenia (Bray, Gunnell, & Smith, 2006), but I was aware of aging’s effect on chromosomes already so that potentiality was easily grasped. I have little knowledge of long term epigenetic effects of obesity. Very interesting!
ya!!! it is very fascinating topic to discuss and know more about paternal obesity and its role in trans generation impact. There is a special was so curious about this point of discussion was , i always come across many woman who suffer , embarrassed,victimized due to obesity especially when it comes to infertility,child birth and and obesity. The recent study The researchers found evidence that obesity changes the microRNA (miRNA) signature—epigenetic regulators of gene expression—in both the dad’s sperm and the daughter’s breast tissue, suggesting that miRNAs may carry the epigenetic information from obese dads to their daughters. [The miRNAs identified regulate insulin receptor signaling, which is linked to alterations in body weight, and other molecular pathways that are associated with cancer development such as the hypoxia signaling pathway](https://gumc.georgetown.edu/magazine/2016/fall-winter/paternal-obesity).
I agree with you Shane, but what really strikes me is the longevity of the effect. We have understood for a while the negative consequences of drug use and smoking cigarettes while pregnant but most people don’t think of the extra few pounds they carry around in the same manner. We are learning through continuing research just how detrimental having extra body fat can be, in this case even in pregnant mothers.
It would be advantageous for potential mothers looking to become pregnant to have an exercise regimen as well as a healthy diet, aiming to be as lean as possible before pregnancy in order to counter this effect. As most pregnant women can attest, continuing to move and stay active is difficult during pregnancy, but has far reaching positive benefits for both baby and mother. If a mother begins pregnancy overweight, it becomes increasingly difficult to get it off during this time. As illustrated in this post, this excess weight has a large negative effect on the immune system of the newborn. There are studies that show that it also has long term negative effects upon digestion and metabolism. This makes it a cyclic issue as it becomes possible that an obese mother has a female child predisposed to obesity that then perpetuates the cycle by becoming an overweight mother herself. (Matthew W. Gillman, M.D., and David S. Ludwig, M.D., Ph.D.
How Early Should Obesity Prevention Start?
December 5, 2013
N Engl J Med 2013; 369:2173-2175)
Besides the risk of giving birth to a baby with immune insufficiencies, new research has surfaced stating the babies who are born through cesearan sections are at risk of having asthma and food allergies. It is stated that vaginal births expose the infant to pathogens that kickstart the immune system and its ability to create immune memory, which is great for a developing baby. Unfortunately, as Dr. Putnam stated in her article, “obese pregnant patients are more likely to have elevated blood pressure, gestational diabetes and babies with birth complications.” But she also stated that “they are more likely to need cesareans.” Therefore, being obese as a pregnant patient puts you in a predisposition to have a cesarean section. If obesity continues to be a trend seen in pregnant women and C sections become the norm, then we will soon see more immunodeficiencies than ever before.
Boutsikou, T., & Malamitsi-Puchner, A. (2011). Caesarean section: impact on mother and child. Acta Paediatrica (Oslo, Norway: 1992), 100(12), 1518-1522. doi:10.1111/j.1651-2227.2011.02477.x
Quentin, I found your comments to be very interesting. I was born through a Cesarean section, not due to maternal obesity, but because I was breeched. I never thought that being born of a C-section can predispose the fetus to complications that they may not have encountered if born through a vaginal birth. Also, I was unaware that obese mothers are more likely to need Cesareans. There was a study done in New York over a 3 year period from January 2010 to December 2012 to determine a connection between obesity and Cesarean section births. Women were classified as underweight, normal, overweight, and obese levels I, II, and III. Results were collected on 2155 women with 29% having obese BMI’s. The results showed that infants born to obese mothers are more likely to be delivered by C-section with larger birth weights and infants born to obese level III mothers were more likely to require assisted ventilation and NICU admission. Why is this? According to research, more glucose availability to the fetus causes the possibility of a macrosomic fetus. Macrosomia is a term used to describe a larger than average baby. Glucose levels increase normally towards the end of pregnancy but increase even more in obese mothers. Also, women with high BMI’s tend to have increased inflammation or added soft tissue deposits in the pelvic region. This results in difficulty in delivering the baby due to more contractions and difficulty overcoming the obstruction.
Citations
Khalak R, Cummings J, Dexter S. Maternal obesity: significance on the preterm neonate. International Journal Of Obesity (2005)[serial online]. October 2015;39(10):1433-1436. Available from: MEDLINE with Full Text, Ipswich, MA. Accessed November 12, 2016.
Graham L, Brunner Huber L, Thompson M, Ersek J. Does Amount of Weight Gain During Pregnancy Modify the Association Between Obesity and Cesarean Section Delivery?. Birth: Issues In Perinatal Care [serial online]. March 2014;41(1):93-99. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed November 12, 2016.
Quentin,
This is a great point, and gives all the more reason for physicians to do there best to help mothers who are obese and overweight -since they are at risk of becoming obese-. My nephew has bad asthma and has been to the hospital many times because of complications caused by the illness. Hopefully this approach helps to reduce the obesity population and create a healthier america.
According to the World Health Organization (WHO, 2013) diseases are driven by various factors including the globalization of unhealthy lifestyles. Unhealthy lifestyles can lead to obesity, insulin resistance increased blood pressure, and chronic disease, amongst other things, with a 70 percent chance for the potential of heritability.
There are many factors contributing to the increase of obesity amongst individuals including the industrialization and commercialization of food, individual socioeconomics, and lifestyle choices. Obesity of an individual in itself can bring about many complications, but this article brings out the heritable effects obesity can have on offspring. The offspring are now predisposed to obesity at birth and throughout life, increasing chances for diseases later in life. This article points out the effects that maternal obesity can have on the immunological efficiency of a child.
Before reading this article my initial thought was that of curiosity, wondering how maternal obesity would cause immune system complications in babies, but it makes sense! Hypertension in the mother due to diabetes or an unhealthy lifestyle would have an impact on the fetus because the fetus’s blood is supplied by the mother. If there are increased solutes in the mother’s blood there will be an increase in solute concentration of the child’s blood supply. Cells and proteins found within the bloodstream can be subject to complications because of these and other factors.
Citations
Balogh V. The Consequences of Maternal Obesity. International Journal Of Childbirth Education [serial online]. January 2015;30(1):54-58. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed November 9, 2016.
Hi Sonya,
You made a really good point. The socioeconomic status (SES) of an individual has an impact on their lifestyle. Specifically, in high-income countries, those with lower SES are more like to be obese. The Population Reference Bureau http://www.prb.org/Publications/Articles/2013/obesity-socioeconomic-status.aspx
implied that among white females, all SES groups had a greater risk of obesity compared with the highest SES. Also, among black women, those from working-poor households who now had lower-status jobs were at increased obesity risk compared with the most advantaged group. Unfortunately I think these risks are true. The most advantaged SES women do not face the problems that lower SES women face. For example, lower SES women most likely have to obtain a job to support their families and live comfortably. Therefore, they may not have time to cook and/or exercise. These women probably decided to eat out more times than not. Also, among those that have financial issues, fast food is so affordable and convenient that they settle for these restaurants to meet their nutritional needs.
Pregnancy and lactation is the time woman get fed most in their life span and ‘fed for Two’.This is a wrong idea and practice which is followed for generations all over the world-making a major cause of obesity.During the pregnancy, the quality of the food is more important than the quantity.The health of the mother is crucial for the healthy growth of the baby .There is no chance of dieting or weight loss programs during pregnancy. Hence,women have to make the diet plan and good exercise and make them to be in a good BMI level before conceiving and doctors have to closely monitor the weight gain of the mother and child to avoid the complications like preeclampsia, gestational diabetes, c-section ,premature delivery, impaired immunity of the newborn, type II diabetes,cardiac problems in later age of their life etc.and can fix a diet plan after consulting with a dietitian. Unhealthy lifestyle and stress is the main cause of obesity hence both have to be avoided during pregnancy.
Reference:
http://www.marchofdimes.org/pregnancy/being-overweight-during-pregnancy.aspx.
http://www.babycenter.com/0_having-a-positive-plus-size-pregnancy_1504849.bc
Arya,
I agree with your conclusion regarding this post. Obesity more often than not is a lifestyle problem rather than a purely genetic predisposition. For this reason, it is important to guide expectant mother’s in the right direct for their health and the health of their child. As you mentioned, this should be done prior to pregnancy due to the difficulty of weight loss at the time.
Weight is a sensitive topic for most women. However, the health and safety a woman’s child, makes a weight management conversation more bearable. Most mothers do what’s necessary to ensure their children have a viable future. Therefore, I agree with the statement in the blog about physicians having a discussion about the risks of obesity and the effects it could have on the newborn. In addition to explaining the risks, a treatment plan should be created to reduce the BMI in the mother.
According to the article in the Sunday Review of the New York Times, Pregnant, Obese…and in Danger, obese and overweight pregnant women are more like to have an obese or overweight child. The American Heart Association warned that these obese kids face adult problems like high blood pressure, type 2 diabetes and high blood cholesterol levels. These health problems can lead to chronic health problems that may require surgery, such as atherosclerosis. The AHA also advises that obese children face low self-esteem, depression, and self-loathing. I believe that if obese pregnant women knew they were putting their children’s health in jeopardy, then they would be open and motivated to hear the doctor’s recommendation. All newborns deserve to get the best start in life.
Another good reason why the Ob/Gyn should disclose the risk factors associated with being pregnant and obese is the complications that the mothers face during labor. The birthing complications could lead to a longer recovery time and thus more expenses for the patient. These pregnant women become susceptible to diseases too. Some obese pregnant patients develop gestational diabetes and high blood pressure. Therefore, I absolutely think it is in the best interest of the doctor to offer preventive care of such disease and subsequently lower the need for major surgery, such as a cesarean as discussed in the blog. The doctor should offer preventive care by means of a weight loss plan.
American Heart Association: http://www.heart.org/HEARTORG/HealthyLiving/HealthyKids/ChildhoodObesity/Overweight-in-Children_UCM_304054_Article.jsp#.WCOhq_mAOko
Obviously there is a direct correlation between the health of a mother and the health of the baby she is carrying and substantial evidence of a correlation between obesity and health. There is substantial evidence to demonstrate a relationship between obesity and negatively impacted immune systems and this paper goes beyond that to delineate relationships at the cellular level. The next step is research into potential molecular mechanisms at work as well as research validating what has been found here. I found the choice to use BMI instead some other measure of visceral fat as my understanding is that visceral fat is the key component to why obesity is dangerous and that BMI is a highly flawed metric (Rothman, 2008). I found the application of a high fat diet on the murine subjects interesting also, as high fat diets have been shown to inhibit innate immunity (Pizzola et al, 2016). I’d like to see research that determined whether the diet of the mother or the visceral fat percentage of the mother was responsible for the compromised immune systems found in their offspring. Would a child born to an obese mother who nevertheless consumed a low fat high fiber diet while pregnant show the same compromised innate immunity found here? Arguably there’s low potential public health benefit to such research, there’s a kind of circular logic in that obese people generally consume unhealthy foods and people with a healthy body fat composition generally do not, so really how much of the population could be served in finding out if it’s being fat or acting fat that’s responsible for the negative health effects here? At the same time from personal observation it does seem that pregnancy can spur significant changes in diet (both positive and negative) so further research on that question could be beneficial.
Citations
Pizzolla, A., Oh, D. Y., Luong, S., Prickett, S. R., Henstridge, D. C., Febbraio, M. A., & … Hardy, C. L. (2016). High fat diet inhibits dendritic cell and T cell response to allergens but does not impair inhalational respiratory tolerance. Plos ONE, 11(8), 1-18. doi:10.1371/journal.pone.0160407
Rothman, K.J. (2008). BMI-related errors in the measurement of obesity. International Journal of Obesity (2008) 32, S56–S59; doi:10.1038/ijo.2008.87
James, I really enjoyed reading your response. You asked a lot of questions really drilling down at what might otherwise be arbitrary metrics used not only in the study referenced in this blog, but often across several others studies I’ve already looked at. It does seem like a question that might devolve into circular logic, however, there are indeed times when obesity is caused by issues not directly related to the amount of fat consumed. In fact, I’ve come across several studies that have linked obesity to malfunctioning immune systems. Funny enough, one study wasn’t even intentionally trying to find a link between obesity and the immune system, but was studying autoimmune disorders. But after genetically engineering out dendritic cells that use perforin, they were surprised to see their mice had developed metabolic problems, showed signs of insulin resistance and heart disease, and gained weight. The second study linking obesity to a faulty immune system is actually a review looking at studies tying adipose tissue inflammation and consequential insulin resistance. Given that obesity and a high fat diet can actually be mutually exclusive, I must agree that studies should be careful in defining the conditions being altered for study as to better distinguish what specific health factors are contributing to these embryonic phenotypes. Granted, I doubt neither obesity nor a high fat diet are likely to be healthy for the offspring based on all the studies I’ve looked at related to this blog.
Citation: Zlotnikov-Klionsky Y, Nathansohn-Levi B, Shezen E, et al. Perforin-Positive Dendritic Cells Exhibit an Immuno-regulatory Role in Metabolic Syndrome and Autoimmunity. Immunity. 2015;43(4):776-787. doi:10.1016/j.immuni.2015.08.015.
Citation: Shu CJ, Benoist C, Mathis D. The immune system’s involvement in obesity-driven type 2 diabetes. Seminars in Immunology. 2012;24(6):436-442. doi:10.1016/j.smim.2012.12.001.
Yeah I’m not sure how much of a difference it would actually make in terms of what a doctor would tell the patient, I would imagine the range of potential approaches to treating obesity is considerably limited if the patient is pregnant, but if the mother is of a healthy weight and the causal agent here is tied specifically to the diet during pregnancy it would be useful to know.
Not to beat this with a stick, but I just read an interesting article suggesting that certain infections can actually lead to obesity (1). They are calling it “infectobesity,” In the article, it states that bacterial endotoxins can surprisingly cause the expansion of adipocytes. Immediately, I started wondering how this could be beneficial to the bacteria itself, but then I realized that having a high BMI, lowers the chance of starvation. Thus, making us longer- lasting hosts. This then puts everything into a sequela of events. An acquired infection leads to obesity, which then leads a weaken immune system. Finally, children born to obese mothers acquired obesity and immune fragility themselves. Ultimately, it’s a vicious cycle.
Citation:
1. Hegde V, Dhurandhar N. Microbes and obesity–interrelationship between infection, adipose tissue and the immune system. Clinical Microbiology And Infection: The Official Publication Of The European Society Of Clinical Microbiology And Infectious Diseases [serial online]. April 2013;19(4):314-320. Available from: MEDLINE with Full Text, Ipswich, MA. Accessed November 13, 2016.
The mother’s influence on her child does not start at birth, but much sooner than then as this blog post and Wilson’s paper demonstrate. The adverse effects of maternal negligence in the realm of tobacco, alcohol, drugs of abuse have long been established. However, as this blog post points out, less talked about form of harm can be as dangers on the vitality of a newborn both in the acute and chronic sense. I am interested in understanding the underlying mechanisms influencing the observed changes between mothers with normal and obese BMI, respectively. Elshenawy et al partially answered the questions in their discussion of prenatal preprogramming via epigenetic cues. Epigenetics is the change, modification, and regulation of gene expression rather than the underlying genetic code. Their study focused on fetal programming by maternally obese individuals. Most interestingly, this research could lead to novel strategies for treating transgenerational obesity and its associated complications.
Citations:
1. Elshenawy S, Simmons R. Maternal obesity and prenatal programming. Mol Cell Endocrinol. 2016 Nov 5;435:2-6. doi: 10.1016/j.mce.2016.07.002. Epub 2016 Jul 5.
This a well know topic that maternal obesity has a negative outcome on the fetus. As discussed in the post, Doctors should talk about weight and weight management as it relates to both the mother’s and the child’s health. Physician’s should also speak about breastfeeding early on in pregnancies. Nearly one fifth of women giving birth in the United States are obese. Women with obesity are less likely to breastfeed and are more likely to cease breastfeeding earlier than their normal weight counterparts. Breastfeeding offers some protection for the infant against early rapid weight gain and may promote return to pre-pregnancy weight in the mother.
Infants who are breastfed either directly at breast or by receiving breast milk in a bottle have a better health outcomes including lower risk for otitis media, gastroenteritis, obesity, and sudden infant death syndrome. Human milk protects against infections in the breastfed offspring mainly through secretory IgA antibodies, but also most likely through several other factors like the bactericidal lactoferrin. Breastfeeding has been associated with lower risk for type 2 diabetes mellitus, the metabolic syndrome, postpartum depression, and cardiovascular disease in mothers. Maternal obesity and lack of breastfeeding interact to robustly increase risk for later obesity in the offspring. Breastfeeding decreases risk for later obesity in infants. In the baby, breastfeeding promotes optimal feeding because infant demand is matched to milk production in the mother. This helps to avoid infant overfeeding. Formula-fed babies have been shown to have higher risks for obesity and type 2 diabetes mellitus. Open dialogue about breastfeeding can lead to educating parents about the additive benefits for the mother and child.
Citation:
1.Williams, C. B., Mackenzie, K. C., & Gahagan, S. (2014). The Effect of Maternal Obesity on the Offspring. Clinical Obstetrics and Gynecology, 57(3), 508–515. http://doi.org/10.1097/GRF.0000000000000043
2. Breastfeeding Provides Passive and Likely Long-Lasting Active Immunity
Hanson, Lars A
Annals of Allergy, Asthma & Immunology , Volume 81 , Issue 6 , 537 – 534
http://www.annallergy.org/article/S1081-1206(10)62704-4/pdf
3.http://digitalcommons.brockport.edu/cgi/viewcontent.cgi?article=1090&context=honors
Obesity has very negative effects on the health of women. Obese women have a higher risk of diabetes, coronary heart disease, low back pain and knee osteoarthritis. Contraception and fertility are also negatively affected. Studies (1-3) have shown that maternal obesity is also associated with a decreased intention to breastfeed, decreased initiation of breastfeeding, and decreased duration of breastfeeding. Other studies (4-5) show that there is an association between obesity and depression in women. Obese women are also at higher risk for multiple cancers.
Maternal obesity is linked with higher rates of cesarean section and pregnancy outcomes are also negatively affected as there is increased risk of neonatal mortality and malformations. I found it pretty surprising that the rates for antenatal detection of fetal anomalies have been shown to be significantly decreased in women with a BMI of 30 or more when compared with women whose BMI falls within the recommended range. Once they are born, these children face increased risks of obesity and hypertension in adult life, supporting the findings that the intrauterine environment can affect the health of children.
In order to manage obesity in pregnant women, BMI should be calculated for all women. Women should be counseled on physical activity, and a dietary and nutritional assessment should be undertaken, including an assessment of both obesity and eating disorders. Physicians play an integral role in making recommendations to promote behavior change for women who are obese or at risk of obesity.
Citations:
1. Hilson JA, Rasmussen KM, Kjolhede CL. High prepregnant body mass index is associated with poor lactation outcomes among white, rural women independent of psychosocial and demographic correlates. J Hum Lact 2004; 20: 18–29.
2. Li R, Jewell S, Grummer-Strawn L. Maternal obesity and breast-feeding practices. Am J Clin Nutr 2003; 77: 931–6.
3. Oddy WH, Li J, Landsborough L, Kendall GE, Henderson S, Downie J. The association of maternal overweight and obesity with breastfeeding duration. J Pediatr 2006; 149: 185–91.
4. Onyike CU, Crum RM, Lee HB, Lykestos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 2003; 158: 1139–47.
5. Ross CE. Overweight and depression. J Health Soc Behav 1994; 35: 63–79.
There has been studies that show genetics plays a determining factor as to whether or not a child becomes obese. But I personally believe that environment (in terms of the food consumed) plays a greater role in the risk of a child becoming obese. It has been said that not only are genetics inherited by the parent but also their eating habits. But all in all, helping the parent manage their weight should help prevent the risk of the child developing obesity in both aspects. So I support the idea of physicians making suggestions to help pregnant mothers control their weight prior to the child’s birth.