Climate change is expected to significantly influence the geographical distribution and impact of infectious diseases worldwide, especially those that require vectors such as mosquitoes and ticks for transmission. However, undernutrition has been identified as the greatest effect of climate change on health.
Results from a study published last year in the Proceedings of the National Academy of Sciences, give a different perspective to this problem. The study (High ambient temperature dampens adaptive immune responses to influenza A virus infection) examines how high temperatures and subsequent reduced food intake affect the adaptive immune response to influenza virus infection.
The researchers housed healthy, young adult female mice in different temperature conditions—a group of mice was kept at refrigerator-cold temperature (4 degrees Celsius or 39.2 degrees Fahrenheit), another group at room temperature (22 C or 71.6 F), and an additional group at high-heat (heat wave) temperature (36 C or 96.8 F). The researchers then infected the mice in the different groups with the influenza virus, and compared their immune responses.
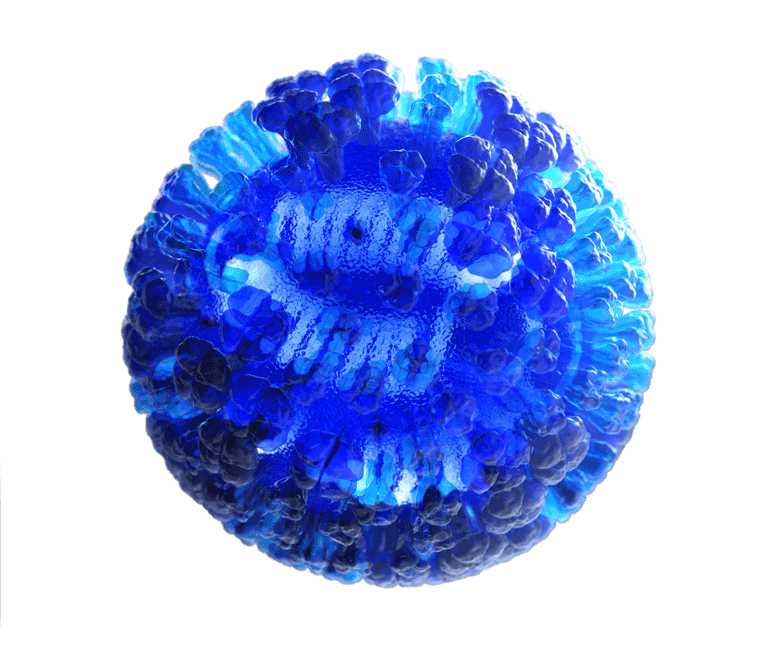
The researchers found that, compared with mice kept at room temperature, high heat-exposed mice reduced their food intake and exhibited a 10% reduction in body weight, although commensal microbiota composition remained intact. In addition, high heat-exposed mice developed impaired immune responses to the influenza virus— these mice failed to stimulate inflammasome-dependent cytokine secretion and migration of respiratory dendritic cell to lymph nodes, and exhibited increased autophagy in lung tissue. In room temperature-exposed mice, induction of autophagy severely impaired virus-specific CD8 T cells and antibody responses.
Heat exposure also impaired immune responses in mice infected with either Zika virus or a pathogenic tick-borne phlebovirus that causes severe fever with thrombocytopenia syndrome. Injection with either glucose or dietary short-chain fatty acids (which are metabolites produced by gut microbes) restored influenza virus-specific adaptive immune responses in high heat-exposed mice.
These findings suggest that outside temperature and host nutritional status may be critical determinants of viral pathogenesis or vaccine efficacy. People often lose their appetite when they feel sick. If someone stops eating long enough to develop a nutritional deficit, that may weaken the immune system and increase the likelihood of getting sick again.
Takeshi Ichinohe, one of the two study co-authors, said in a press release: “People often lose their appetite when they feel sick. If someone stops eating long enough to develop a nutritional deficit, that may weaken the immune system and increase the likelihood of getting sick again.” He added: “Perhaps vaccines and nutritional supplements could be given simultaneously to communities in food-insecure areas. Clinical management of emerging infectious diseases, including influenza, Zika, and Ebola, may require nutritional supplements in addition to standard antiviral therapies.”
As the child of parents from Nigeria, it was of no surprise to me when I learned that people in areas more prevalent with malnutrition can have weaker immune systems. Life is about growing both physically and mentally. Just as we grow each day, our cells need nutrients and other substances that help them grow.
Prior to reading this article however, I did not fathom how this malnourishment could effect cells within the immune system. In order to find out more how the immune system and body is changed when someone is malnourished, I read this article, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527386/.
In this article, the author states in areas such as Africa, Asia, and South America where nutritional defects are more prevalent, those who are malnourished are more at risk for infections. Those who have malnutrition are more likely to have dysfunctions within their mucus membranes, as well as a lower number dendritic cells in circulation which not only present viruses, but are the bridge between the innate and adaptive immune system. The article mentions that B-cells, which also present pathogens, are in lower numbers however, the number of immunoglobulins such as IgG and IgM remain unaffected. IgA which is an immunoglobulin found commonly in the mucosal layer tends to be more elevated in individuals with malnutrition (which makes sense since they have less cells here).
This peer reviewed article and the blog both illuminate the unintended consequences that can result from malnutrition. In order to effectively utilize and eradicate the world of viruses and diseases, further study in areas more plagued with nutritional deficiencies will be important at preventing subsequent infections in the future. As a novice immunologist myself and aspiring scientist, I know the wonder vaccines and vaccine access can do for those in need of help however, a lack of resources and poverty can prevent one from ever truly being cured.
I agree, when we think of climate change we tend to only focus strictly on the environmental consequences and not how it can influence our health, specifically our immune system. I found another study similar to the one you mentioned that found that malnutrition can lead a decrease in the number of antibody secreting cells (b-cells) and that this can alter the efficacy of vaccines. Since human rotavirus (HRV) is the leading cause of child mortality in developing countries, the researchers examined how malnutrition effected the immune response prompted by the HRV vaccine. They exposed newborn pigs either sufficient or deficient milk diets and vaccinated them twice at a 10-day interval. They found that HRV-specific IgG and IgA antibody secreting cells (ASCs) were reduced in blood or intestinal tissues the vaccination in the pigs that were exposed to the deficient diet. I think this finding is particularly important because it stresses the importance of the whole person approach in medicine. Like you mentioned in your comment, if we truly want to cure diseases it is absolutely imperative that we also look at the underlying issues.
https://www.ncbi.nlm.nih.gov/pubmed/32117313
I can definitely agree with your statement on how regions such as Africa, Asia, and South America have greater risk for infections due to low food availability. However, the climate that makes up these regions can also affect them at a disproportionate rate when it comes to several diseases. For instance, in Iran there has been a history of outbreaks of cholera disease throughout the region. The climate here is hot and wet which provides a comfortable environment for this disease. Climate change has been conveyed to cause outbreaks of several water-borne diseases. In a recent article, it projected the climate to experience lower precipitation and higher temperatures. The study found a direct correlation between low precipitation and cholera infection. Particularly in warmer months, the combination of low precipitation and high temperatures could make for swifter replication of the bacteria. This would put individuals living in this region at a disadvantage because if exposed, the bacteria are able to work faster in a person residing here versus a member of another climate. The immune system will have to fight harder and the infection will last longer due to the change in climate allowing the infection to replicate more efficiently.
Asadgol, Z., Mohammadi, H., Kermani, M., Badirzadeh, A., & Gholami, M. (2019). The effect of climate change on cholera disease: The road ahead using artificial neural network. PloS one, 14(11).
I find this article very interesting because climate is a factor I wouldn’t typically consider when thinking of human gut microbiome composition. On the other hand, I’ve always heard that majority of the human immune system is provided by the microbiota of the gut. Therefore, a large part of what we eat differs depending on the season, so it appears to be a full circle. Also, as noted in the article, with high temperatures, it’s been discovered that humans tend to consume less food. Personally, I feel this could be attributed to fact that our bodies are able to maintain a state of homeostasis in temperatures closer to our core, cutting out the need for additional work, hence less calories are needed. The articles states that a decrease in caloric intake could cause harmful alterations in the gut microbiota, leading to an impaired immune response. This indicates that temperature is a key controller in the pathogenesis of certain viruses. This is slightly concerning because temperature is not always a factor that can be controlled and eating when you’re not hungry has been known to have a few undesirable effects on the scale. In addition to the effects of temperature change that come with season change on gut bacteria, season change also brings illnesses that can cause depletion of healthy bacteria. In a recent article I found, I learned that though the gut microbiome is of the most diverse, there are two major categories of microbes in the human gut: autochthonous microbes and allochthonous microbes. Autochthonous microbes are found on the epithelium of colonic mucosa while Allochthonous microbes are found passing through the lumen during digestion. These two categories have various functions, but their ratio to each other is believed to be a major player in a diseased state vs healthy state and in screening for various diseases such as cirrhosis progression. In warmer environments, infections caused by Allochthonous microbes are more abundant than in cooler climates. The article also makes suggestions for combating deficiencies in the gut microbiome. A type of microbiome manipulation was introduced involving a cocktail of prebiotics, probiotics, and synbiotics. This could be very beneficial during times of poor dietary habits or illness. These cocktails include species such as gram-negative bacteria, which are found in abundance in the health gut microbiome. These bacteria have been cited as strong stimulators of innate immunity. I would like to further research this topic to determine if through manipulation of body temperature, we could also induce an abundance of specified microbial growth leading to a forced state of health. Could the temperamental effects of temperature also be manipulated to work in our advantage?
Reference
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5785832/
The findings in this post are quite alarming to me because I know that there has been a continuous increase in temperatures worldwide due to the effects of climate change. The results that the researchers found using the mice are just as likely to happen in humans because their immune systems will not be able to function properly due to high temperatures and their lack of nutrition. A recent study in 2019, further supports the findings that climate change negatively affects both animals and humans’ immune systems. Researchers also found that heat stress causes a decrease in food intake, resulting in a deficit in nutrition that livestock need. The heat stress also caused a reduction in the volume and weight of lymphoid organs, thus leading to lower levels of immunoglobulins and reduced phagocytosis. This also hinders their bodies from having the proper immune responses. It is essential for the inhabitants of the world to understand that climate change plays a significant role in the immune systems of both animals and humans, which should give more reason as to why the issue of climate change needs to be addressed and prohibited.
Reference : https://www.ncbi.nlm.nih.gov/pubmed/32083100
After reading through the post, I was intrigued by the study showing that warmer temperatures associated with climate change actually affect the immune response. It was interesting to see that the research presented was specific to the adaptive immune response in mice, which brings the question if the innate immune response could possibly be impacted in a similar way.
The information explained in the post also made me inquire whether or not there are other climate related factors that could alter immunity and if so, what makes these cases different. A research study observed the potential effects of aridity, or the dryness of air, on the habitat of a West African bird species known as Pycnonotus barbatus. Prior to testing immune indices in the birds, the scientists believed that if the inhabited environment was more arid, then the innate immune response would be negatively affected. The increased aridity was associated with a loss of the food supply due to the dry conditions, which made the scientists believe lack of food correlates to a higher number of infections. The researchers observed specific immune indices: haptoglobin, the concentrations of nitric oxide and ovotransferrin, and haemagglutination and haemolysis titres in the blood. These indices do many things to fight against infection– haptoglobin and ovotransferrin work with inflammatory responses, and nitric oxide is a molecule that works to kill parasites. Haemolysis titres and haemagglutination function between innate and adaptive immunity to ultimately fight off pathogens with antibodies. Unfortunately, inconsistencies were found within the study, and there appeared to be no difference in the immunity of any of the bird species. This now brings the question of how to figure out which specific components will impact the immune system in terms of climate change. It personally was surprising to see that the results were not very similar to that of the increased temperature study, since dry air can be associated with higher temperature. Even though both studies were testing for the same thing, it is important to remember that they are not identical. One difference between these two experiments was the category of immunity being observed. There must be more work to be done in determining which factors could be altering the specific aspects of immunity, as well as different species of organisms, and their environments.
Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7125124/
To reply to your inquiry, another climate-related factor that is affecting our immune system is UV radiation. As temperatures continue to increase, so does UV radiation from the sun. Upon my research, I found in an article, Human Health in Relation to Exposure to Solar Utraviolet Radiation Under Changing Stratospheric Ozone and Climate, that states UV exposure can lead to skin cancer, psoriasis (an autoimmune disease), multiple sclerosis (an autoimmune disease), and many other conditions. Each of these ailments listed directly affects the immune system. For example, cancer weakens the immune system as a whole. Autoimmune diseases like psoriasis and multiple sclerosis alter the immune system to attack healthy cells and itself. Therefore, the same way climate change is affecting our immune system so is UV radiation.
Furthermore, the article discusses how the incidence of skin cancer is increasing in lighter skin populations. Not only is UV radiation increases as climate increases, but it is also targeting a specific group of people. This can be very alarming to individuals within that target population. However, there are preventative measures that can be taken, such as sunscreens and clothes, as the article suggests. Everyone must take precaution on how the climate is affecting our bodies and immune system.
https://www.ncbi.nlm.nih.gov/pubmed/30810559
The pervasiveness of this issue means that the potential solutions must be multi-faceted. In other words, if the problem is caused by many factors, then the solution must be designed to address all these problems, otherwise the problem will not truly be solved. This is touched on near the end of the post, when one of the study authors mentions the concept of giving both vaccines and nutritional supplements to food insecure areas. This specific comment made me consider how malnutrition affected not only the body’s immune response, but also its response to vaccines. In researching this, I cam across a study that was performed on Gnotobiotic pigs to measure how their nutrition affected their responses to HRV vaccination. In these experiments, it was noted that subjects that had received a deficient nutritional value, subsequently produced a deficient number of HRV specific IgG and IgA antibody secreting cells. So it appears that while attempting to rectify the problems caused by climate change induced malnutrition, immunologists would have to consider the long term effects of malnutrition and how those effects have to be treated and reversed over a longer period of time before the patient’s immune system returns to fully functional levels.
Source:
https://www.ncbi.nlm.nih.gov/pubmed/32117313
Hey Jordan,
This perspective is very valid, the concept of handling issues like this can be handled by taking more than just one measure to solve them. After reading through the article posted however, I was interested to see that the Human Rotavirus virus was not impacted directly by the lack of nutrients in the pig models, but more on the antibodies that fight against infection in the immune response. I was curious to figure out what other aspects of the immune system that virus was a part of. I came across an article entitled “Human Rhinoviruses” discussing how the virus has impacted both the innate and adaptive immune system response. The immune system recognizes the virus with various toll receptors, also known as TLRs (TLR2, TLR7, and TLR8 for example) and once the the virus is incorporated in the genome, RNA molecules and interferons (signalling proteins that work against infection within the immune system) are generated to fight against the virus specifically. With HRV, the interaction with TLRs as well as the cascade of responses following this cause an increase in the production of the cytokines–specifically IL-8. The heightened production of this cytokine is clinically connected to a common symptom of infection in epithelial cells in the upper and lower airways within the body. The immune system essentially stimulates the spread of the virus through cytokines and interferons specifically, which causes persistence of infection.
Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3553670/
Judging how warm it was this past winter, I’m sure climate change is on the rise. We always hear how climate change will affect us environmentally, such as rising sea levels and temperature, crops not being able to grow, etc. but, we never hear how it’ll bring on the rise of more pathogens. From a peer-review article by Mirsaeidi et al., there have been many reports of outbreaks of diseases due to climate changes such as the hantavirus outbreak in Panama in 99-00. Recent studies show that if climate changes continue, respiratory infection rates will increase. Climate changes will change wildlife habitats and bring them into closer contact with humans bringing with them diseases we usually don’t have immunity too or regularly exposed too. More intimate contact with wildlife would also mean a higher chance of zoonotic diseases to occur. Vector-borne diseases also thrive in warmer weather increases the risk of malaria, West Nile virus, and cholera.
Reference:
https://www.ncbi.nlm.nih.gov/pubmed/27300144
The consequences of climate change are neither rectifiable nor preventable; this is to say that we must accept and adjust to its realities. Living in the Anthropocene, global temperatures are expected to rise. I find that this increase puts impoverished countries at higher risk for disease due to the double-pronged problem of limited access to medical resources and food scarcity. Though health professionals recommend maintaining a healthy and consistent diet comprised of essential nutrients and minerals, this is virtually an unobtainable feat to uphold worldwide. As a potential solution, I would encourage further research promoting the genetic engineering of certain foods to enrich nutritive and immune-boosting content in a replicable and sustainable manner. Though not a novel concept, prior attempts at doing so, such as hepatitis B-anana and golden rice, have not proven reliable for several practical reasons. Some challenges with creating these plant-based superfoods are providing long-term evidence that supports high crop yield for little cost, possessing high tolerance against harsh environmental conditions, and resistance to spoilage. Surmounting these problems is critical for destitute countries suffering from undernutrition and immunocompromised diseases induced by climate change because it may assist in providing a more stable and accessible food supply. To combat the human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) issue prevalent in several countries, a study published by Molecules (Tuning of the Amount of Se in Rice (Oryza sativa) Grain by Varying the Nature of the Irrigation Method: Development of an ICP-MS Analytical Protocol, Validation and Application to 26 Different Rice Genotypes) aims to improve the process of optimizing nutrient enrichment through genetic modification (GMO) in a more efficient way. Enhancing O. sativa, commonly referred to as Asian rice, with selenium, serves a dual purpose; it regulates metabolism and slows the progression of HIV into AIDS. Thus, by being a nutritional food source and bolstering immune defense, populations may benefit from consuming this product.
https://www.ncbi.nlm.nih.gov/pubmed/32316646
The consequences of climate change are neither rectifiable nor preventable; this is to say that we must accept and adjust to its realities. Living in the Anthropocene, global temperatures are expected to rise. I find that this increase puts impoverished countries at higher risk for disease due to the double-pronged problem of limited access to medical resources and food scarcity. Though health professionals recommend maintaining a healthy and consistent diet comprised of essential nutrients and minerals, this is virtually an unobtainable feat to uphold worldwide. As a potential solution, I would encourage further research promoting the genetic engineering of certain foods to enrich nutritional and immune-boosting content in a replicable and sustainable manner. Though not a novel concept, prior attempts at doing so, such as hepatitis B-anana and golden rice, have not proven reliable for several practical reasons. Some challenges with creating these plant-based superfoods are providing long-term evidence that supports high crop yield for little cost, possessing high tolerance against harsh environmental conditions, and resistance to spoilage. Surmounting these problems is critical for destitute countries suffering from undernutrition and immunocompromised diseases induced by climate change because it may assist in providing a more stable and accessible food supply. To combat the human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) issue prevalent in several countries, a study published by Molecules (Tuning of the Amount of Se in Rice (Oryza sativa) Grain by Varying the Nature of the Irrigation Method: Development of an ICP-MS Analytical Protocol, Validation and Application to 26 Different Rice Genotypes) aims to improve the process of optimizing nutrient enrichment through genetic modification (GMO) in a more efficient way. Enhancing O. sativa, commonly referred to as Asian rice, with selenium, serves a dual purpose; it regulates metabolism and slows the progression of HIV into AIDS. Thus, by being a nutritional food source and bolstering immune defense, populations may benefit from consuming this product.
https://www.ncbi.nlm.nih.gov/pubmed/32316646
I like the way that you looked at the global warming situation with such realism-basically saying “it’s already happening, so now we need to adjust to it”. I think it was interesting that you chose to look into genetically modified foods as part of the solution to solidifying the world food supply as many have before you. This subject of genetically modified organisms being used to boost crop production is surrounded by discussion and controversy about possible health concerns. I was curious if by trying to address a problem (world hunger) that was brought up because of immunological/health concerns if we would end back up at more or different health concerns so I looked into the effects of GMO’s. In another article that I found, https://pubmed.ncbi.nlm.nih.gov/26536836/?from_term=gmo+health&from_pos=5, the author states that scientific reports have shown no harm from GMO consumption so far. Many people are still concerned with possible health effects on a long-term time table that have not been seen yet or with how the use of GMO’s may impact pesticide resistance. Another topic of focus is with proper GMO food labeling as many people are concerned with knowing exactly what they are eating, however, I would argue that the average person is completely oblivious to numerous other questionable additives and chemicals they ingest in properly labeled non-GMO foods already.
Reference:
B;, Yang YT;Chen. “Governing GMOs in the USA: Science, Law and Public Health.” Journal of the Science of Food and Agriculture, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/26536836/?from_term=gmo%2Bhealth&from_pos=5.
It is not a surprise the climate change has a comorbid effect on every aspect of human life and the planet itself. With the rise of global warming and the consistent increase of unhealthy individuals, due to exercise and diet, immunity is greatly affected to. You stated in the article that, “outside temperature and host nutritional status may be crucial in vaccine efficacy and immune response”. This mad me look at the geography of the world where malnutrition and higher than normal climate occurs (https://ourworldindata.org/hunger-and-undernourishment). This data showed that Africa has the highest density of malnutrition and a high density of diseases (Zika, Malaria and Ebola). This information formed the question of, with malnutrition due to obesity skyrocketing in other countries plus increasing levels of climate change year by year, could be seeing a future of more illness and deaths to untreatable diseases? Would we be in a situation where thousands would be unable to recover due to their weak immune system? Researchers have found that with climate related increases in temperature, water borne and toxic-related diseases are on the rise and weakened immune systems (children and elderly) may not be able to fight off this new reality. Source: https://www.ncbi.nlm.nih.gov/pubmed/27300144
Reading the blog post “Climate Change and High Temperatures: Effects on the Immune System.” I understand how climate change and temperatures can affect the immune system of mice. For example, in the blog post, the scientist infected mice with influenza and placed them under different temperature conditions to see what effect it would have on the mice’s immune system. The data showed the mice held under higher temperatures developed impaired immune responses to the influenza virus. After reading the post, I inquired on the question of how temperatures affect our brains. Doing a good amount of research, I found an article called “The Impact of Indoor Air Temperature on the Executive Functions of Human Brain and the Physiological Responses of Body” this article focusses on the effect indoor air temperatures have on the executive functions of the human brain and the physiological responses of the body. For the researcher to conduct this study, they gathered 35 male students who were exposed to 4 air temperature conditions of 18°C, 22°C, 26°C and 30°C in 4 separate sessions. The students were simultaneously asked to take part in the N-back test and their respiration rate were recorded to determine the effect of air temperature. The results from this study showed at a high temperature of (30°C), air temperatures had a profound impact on the student’s heart rate, the accuracy of brain executive functions, and the response time to stimuli. The study concludes by providing favorable indoor air temperature can have a significant effect on physiological responses and cognitive functions.
Reference
Abbasi, Ali Mohammad, et al. “The Impact of Indoor Air Temperature on the Executive Functions of Human Brain and the Physiological Responses of Body.” Health Promotion Perspectives, Tabriz University of Medical Sciences, 23 Jan. 2019, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC6377698/.
This post piqued my interest. We, often, tend to oversee the correlation between climate and health. I work with a pharmacist who just the other day made a statement regarding the COVID-19 pandemic that’s going on and Kemp’s statement to reopen businesses. He made a rebuttal that it would be in better interest to leave businesses closed until we see temperatures rise to the known highs that we see in Georgia every year. This is quite interesting considering the experiment presented above which shows that high temperatures can impair immune responses partially due to lowered nutrition intake. Though this article is not focusing on the ongoing pandemic, I’d like to delve into how different aspects of the climate can affect the immune system. This may vary in relation to the varying natures that come with each pathogen. With a virus such as SARS-CoV-2, there are traits that categorize it as a heat sensitive virus. High temperatures makes it difficult for the virus to survive. Another factor mentioned in this study that can be applied to the experiment above is that any sort of abrupt temperature change can come as a shock to the cardiac and respiratory symptom. Humidity also plays a significant role in affecting the immune system. The continuous breathing of dry air can lead to ineffective mucociliary clearance and slight epithelial damage which renders a person more susceptible to infection by respiratory means. To control the spread and effects seen by certain viruses, we may have to resort to creating artificial environment for those already afflicted to slow the spread. It will be a good idea to obtain details about how a certain pathogen acts in the multiple factors that make up our climate.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7142681/
The climate change is a very severe issue that most people do not really pay attention to. It is no surprise that malnutrition can greatly affect the immune response. The original post is very insightful because most conversations about climate change are always on extreme global temperatures but never on the effect on an individual’s immune response. I would never have thought about the effect climate change would have on the one’s food intake. In the research article I read about the effect of nutrition of immune response, it explains how optimal nutrition status for a well-functioning immune system is highly important in the protection against viral infections. Deficiency in vitamins and trace elements can reduce the body’s resistance to infection because these nutrients help in the support of adaptive immunity mechanisms such as antibody production, lymphocyte differentiation, generation of memory cells etc. Some studies that were discussed in the research article mentioned the importance of vitamin D and how the level of vitamin D in the body is linked to the susceptibility of acute respiratory tract infections.
Reference: https://www.ncbi.nlm.nih.gov/pubmed/32340216