The central nervous system (CNS) controls most functions of the body and mind. It consists of two parts: the brain and the spinal cord. The brain is the center of our thoughts, the interpreter of our external environment, and the origin of control over body movement. Like a central computer, it interprets information from our eyes (sight), ears (sound), nose (smell), tongue (taste), and skin (touch), as well as from internal organs such as the stomach. The spinal cord is the highway for communication between the body and the brain.
The CNS is functionally connected to the immune system — the system that defends us against infectious organisms and other invaders. These two systems interact with each other on the basis of complex mechanisms that require the participation of immune cells and fluids containing soluble immune mediators — both of which need to access the CNS and operate within it.

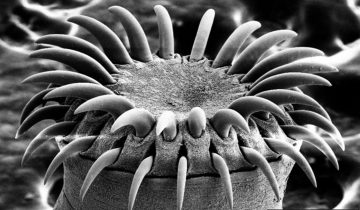
Image credit: Allan Ajifo, CC BY 2.0
The immune system uses lymphatic vessels to exchange immune cells and soluble mediators with tissues and organs, but the CNS does not contain lymphatic vessels. Or, does it?
Here are a few notable examples that illustrate the current view — or, as we will see, an outdated view — on the presence of lymphatic vessels in the CNS. “Lymphatic vessels are not found in CNS tissue”, states an article published in 2003 in Nature Review Immunology. According to an article that appeared in the scientific journal Immunological Reviews in 2006: “It is an undisputed anatomical fact that the CNS lacks a traditional lymphatic system.” A similar statement related to the CNS — “the lack of an obvious lymphatic system” — is present in an article published in 2010 in the Journal of Clinical Investigation. Even a very recent (February 2015) article published in the journal Brain, Behavior, and Immunity, states that “the CNS does not have a well-developed lymphatic system.”
Interestingly, the review authors do not corroborate their statements with references to experimental evidence showing that lymphatic vessels are not present in the CNS. Rather, these statements appear based on “accepted views.” It seems, once again, an instance of the favorite “there is no evidence to show…..”, when the evidence has not been accurately researched. In other words, there is no evidence because no one has been looking — at least systematically — for that evidence. Finally, someone — serendipitously — found the evidence (against the evidence): experimental results published in the journal Nature (June 1, 2015) show that the CNS is directly connected to the immune system by lymphatic vessels previously thought not to exist.
Antoine Louveau, a postdoctoral fellow in the lab of Jonathan Kipnis at the University of Virginia School of Medicine, developed a method to mount a mouse’s meninges — the membranes covering the brain — on a single slide. Thus, the meninges could be examined as a whole. He noticed that immune cells were distributed in vessel-like patterns. Thus, he tested for lymphatic vessels, and he found them. The vessels are able to carry both fluid and immune cells, and are connected to the deep cervical lymph nodes.
So, why were these lymphatic vessels missed by previous investigators? In a press release, Kipnis said that they are “very well hidden” and noted that they follow a major blood vessel down into the sinuses, an area difficult to image. “It’s so close to the blood vessel, you just miss it,” he said. “If you don’t know what you’re after, you just miss it.”
In their paper, the researchers conclude that “Malfunction of the meningeal lymphatic vessels could be a root cause of a variety of neurological disorders in which altered immunity is a fundamental player such as multiple sclerosis, Alzheimer’s disease, and some forms of primary lymphoedema that are associated with neurological disorders.”
Kipnis said in the press release: “In Alzheimer’s, there are accumulations of big protein chunks in the brain. We think they may be accumulating in the brain because they’re not being efficiently removed by these vessels.” Other neurological diseases, from autism to multiple sclerosis, should be reconsidered in light of the presence of something science insisted did not exist.
In addition, Kipnis told The Scientist that, at the very least, these latest results add to mounting evidence of immune activity in the healthy brain. “If you go into the literature, 20 years ago, the idea was that if you see immune cells in the brain, something must be going wrong. Now we know that we see immune cells in healthy brains. . . . It’s part of normal physiology; it should be there. Immune activity in the brain is not always pathological.”
Obviously, the new discovery will point to numerous new avenues of research. However, one of the most important unanswered questions at this time is: “Do these CNS lymphatic vessels exist in humans?”



It is hard to imagine that the brain could exist without its own supply of lymphatic vessels. Immune cells are transported by lymphatic vessels through the body to tissue where they are needed, and the recruitment of effector cells is necessary in the adaptive, prolonged immune response. We also know that immune cells are not only there to protect us against viral agents or infectious diseases, but also to clean up our own dying or dysfunctional cells that undergo apoptosis and can act as “scavengers” of the body. How could it be possible for the brain, a central organ in our functioning, to lack the mechanisms to efficiently remove pathogens and other unneeded cell or soluble remnants? One answer could be that the brain possesses its own set of cells that have immune-like functions and are sentinels of the brain. Another additional layer of protection that the brain possesses is the blood-brain barrier which is there to protect invaders. It could be the collective effort of immune-like cells already present as well the blood-brain barrier but a more likely answer is that CNS lymphatic vessels do exist in humans but have yet to be discovered due to their concealed nature as we have seen with mice.
M.Ilic makes an interesting point in regards to the blood brain barrier, the protective function that it provides against foreign invaders and potentially harmful cells, and the ability of the immune system and the central nervous system to accurately ward of pathological conditions.
When I initially read this statement, it reminded me of Dr. Antoine Louveau’s and Dr. Jonathan Kipnis’s research which they conducted at the University of Virginia School of Medicine. They discovered the Glymphatic System which carries cerebrospinal fluid, a clear substance which surrounds the brain and spinal cord, that carries waste and harmful substances away to be disposed of. The Glymphatic System functions as a series of blood vessels surrounded by channels within the brains of mammals such as mice, and as of recently, even human beings. According to Dr. Louveau and Dr. Kipnis, the Glymphatic System is managed by glial cells. Upon their discovery that vessels carry fluid and immune cells from the cerebrospinal fluid into nearby deep cervical lymph nodes, they deduced that these vessels that help make up the Glymphatic System, serves as a second step in the disposal and drainage of fluid from the brain, after it is drained into the cerebrospinal fluid through the new found Glymphatic System. As stated above, given the fact that this Glymphatic System has also been observed in humans, the next step is to configure the network of vessels in the human central nervous system, assuming that they do in fact exist as stipulated by the aforementioned researchers.
Finally, there is another aspect of the discovery of the Glymphatic System. Disorders and diseases such as immune system dysfunction, multiple sclerosis, meningitis, and Alzheimer’s disease could all potentially be linked to the disruption of the immune cells and their exit from the central nervous system via the Glymphatic System. Dr. Kipnis, one of the researchers that helped discover the Glymphatic System, believes that these vessels within the Central Nervous System may actively play a role in the pathogenesis of the previously mentioned neurological illnesses.
Work Cited:
“Lymphatic Vessels Discovered in the Central Nervous System”. National Institutes of Health. US Department of Health and Human Services. NIH Research Matters. 15 June 2015. Web 27 November 2015. .
It is interesting to see how science evolves and prove it again and again that change is only permanent. It was fascinating to see the journey of the hypothesis of CNS lymphatic system from no lymphatic to poorly developed to well developed. Although the understanding of central lymphatic still incipient, but it will going to help us to understand CNS anatomical structure even better. As per now we still are not sure about the physiological significance of spinal meningeal vessels. Latter is supposed to be lymphatic drainage source for CNS. There is scanty evidence of the connection between central lymphatics and spinal meninges. But above mentioned research seems to be the most probable explanation about the central lymphatic status that how middle man fluid is carried by spinal meninges to peripheral system. Although it is still debatable but hopefully we can uncover the truth with the advent of central lymphatics now. Also, there is some research which hypothesis that drainage of lymph occurs to lateral ventricle from corpus striatum. Although this explanation nullifies the claim of the central lymphatic system. But I feel there may be some middle way from both sides of claims for this middleman of our body. Yet this research really going to explore new avenues for central lymphatics system status.
Reference: 1. Sakka Lauren, Gabrillargues et al 2015. Anatomy of the Spinal Meninges: Neurosurgery. 10. doi:10.1227/NEU.0000000000001048
2. Beatrice Bedussi, Monique G. J. T. B. van Lier, […], and Erik N. T. P. Bakker 2015. Clearance from the mouse brain by convection of interstitial fluid towards the ventricular system: Fluid Barrier CNS. 12:23. doi: 10.1186/s12987-015-0019-5
We must be cautious – even in publications as informal as blog posts – to avoid generalization, mischaracterization and oversimplification, especially when presenting scientific research. The 2003 Ransohoff article (published in Nature Review Immunology) referenced in this blog does not state that there is NO link between the CNS and the lymphatic system, but that leukocyte entry into the CNS is restricted, in large part because of the blood-brain barrier. Given the sensitivity of the brain and potential susceptibility to infection, this barrier is vital to protect the brain from the myriad pathogens that exist in the human body. Ransohoff specifically addressed three routes that leukocytes follow to enter the CNS, via trafficking “signals” (http://www.ncbi.nlm.nih.gov/pubmed/12876559). Another referenced article written by W.A. Banks expands on the role of the blood brain barrier and the fact that the interrelationship between the CNS and immune system is tightly regulated via numerous mechanisms and immunomodulatory molecules, such as cytokines, chemokines, and prostaglandins (http://www.ncbi.nlm.nih.gov/pubmed/25172555).
The author asserts that these studies rely on “accepted views” rather than empirical evidence, yet not only does the Banks article alone cite almost 100 empirical studies, there is an overwhelming body of evidence available that addresses the anatomic relationship between the CNS and lymphatic system (a quick Google search produced 667,000 results, 205,000 of which were linked on the National Institutes of Health website – a respected repository for empirical research). Moreover, while the Kipnis study may raise excitement for enhanced understanding of mouse neuroimmunology with the discovery of lymphatic vessels next to the dural sinuses, one should not leap to conclude the existence of similar structures in human brains. Kipnis’ study includes images of stained macrophages in human meninges and Lyve-1 cells in only 2 out of 9 sampled brains (not an impressive sample size or significant positive finding) (http://www.nature.com/nature/journal/v523/n7560/full/nature14432.html). No human lymphatic vessels were visualized. While the mouse meningeal lymphatic vessels may have been small enough or near enough to blood vessels to be “missed” by the thousands of researchers who have previously dissected mouse brains during experiments, it is difficult to believe that corollary structures in human brains would have been similarly overlooked by all those who have studied human brains. Enhanced imaging techniques certainly will open doors to new discoveries and better understanding of human anatomy, but all new research – no matter how exciting – should still be held to rigorous review for valid and reliable methodology and results.
Finally, while an independent lab visualized similar mouse brain lymphatic vessels, that lab did not include ANY human brains in their study (http://jem.rupress.org/content/212/7/991.long). Moreover, information was presented regarding routes for drainage of CSF that conflicted with Kipnis’ findings. Per Aspelund et al. (citing studies by Kida et al., 1993; Koh et al., 2005; Miura et al., 1998; and Weller et al., 2009), the presence of CSF tracers in the nasal lymphatic vessels under the cribriform plate suggested clearance via olfactory nerve sheaths through the cribriform plate, and CSF clearance has been observed to occur along spinal and cranial nerve sheaths with subsequent entry into extracranial lymphatic vessels (Id). While it would be easy to share in the excitement of newly discovered lymphatic vessels in central nervous system tissue, healthy skepticism should remain until corollary lymphatic structures have been identified in a significant number of human brains, with clear, non-conflicting evidence supporting their functional role.
We must be cautious – even in publications as informal as blog posts – to avoid generalization, mischaracterization and oversimplification, especially when describing the content of scientific articles and contrasting what bloggers report. Being a blogger myself, I see generalizations from the readers occurring frequently.
The author of the blog post says: “[“Lymphatic vessels are not found in CNS tissue”, states an article published in 2003 in Nature Review Immunology.]”
Indeed, the 2003 Nature Review Immunology article does state “Lymphatic vessels are not found in CNS tissue” – you can find this exact sentence on page 571, left column.
I’m very familiar with this 2003 article, having read it over and over a few years ago to write my final undergraduate research report, and I know it is often used to make the point that there are no lymphatic vessels in the CNS tissue.
Do a favor to all of us, and read the 2003 article again, paying attention to it, instead of generalizing and oversimplifying.
Sorry for my stark reply, but I really think everyone should pay more attention when they read.
“a quick Google search produced 667,000 results, 205,000 of which were linked on the National Institutes of Health website – a respected repository for empirical research”
maybe you should try to summarize the 667,000 results, only then you will appreciate that a very small fraction of these results are really related to the topic in question
try to start with the first 100……..
The central nervous system is the part of our body, which controls each and every function starting from the daily normal functions to the complex biological functions in the body. The brain and spinal cord are one of the most vital organs of the system, which controls, receives and delivers signals for many important processes in the human body. The immune system is not an exception, the proper functioning of immune system is also highly dependent on the signals of CNS. The triggering signals from the brain is essential for the production of cells and molecules of the immune system, in order to keep ourselves healthy.
It was always amazing to learn to learn the brain being such a vital organ, it itself does not has any draining lymphatic vessels rather it is directly related to the immune system in order to protect itself. I always used to wonder come this is possible, at last brain is also prone to many infections and diseases. As always said change is the only thing that remains unchanged, it is good to know that there are presence of lymphatic vessels in the brain and it is hidden inside along with the major blood vessel that flow to the sinuses. The way the study was conducted by keeping the meninges along with the skull cap and retaining its physiological condition is really fascinating.
But it is also obvious that this has only been seen in the mouse meninges and not yet been proved in the humans. But it is also to be noted that almost all the new discoveries be it any drugs, pathways or any other physiological changes all of them has been noted first in mouse or any other closely related organisms. Most of them have been obvious in humans too. So taking this into account we can conclude that there are more possibilities for new discoveries in immunology and medicine for many neurological disorders and brain infections. We can also look forward for some new inventions in imaging techniques.
References:
1. http://newsroom.uvahealth.com/about/news-room/missing-link-found-between-brain-immune-system-with-profound-disease-implications.
2. http://www.nature.com/nature/journal/v523/n7560/full/nature14432.html.
I couldn’t agree more with one of the previous comments. While it is easy to become excited with seemingly new breakthroughs in science that contradict our current understanding, caution must be exercised. As the commenter pointed out, there is a multitude of research corroborating our previous assertions that there is limited immune activity occurring within the central nervous system and it is tightly regulated by the blood brain barrier (Banks, 2015). And for good reason as our brain is perhaps our most sensitive organ. Furthermore the research article that this post is based on was unable to yield consistent results or to apply them to the human CNS (Louveau et al., 2015). Before embracing this new idea, further research must be done as decades of empirical scientific research must be overcome.
Perhaps even more disturbing here, however, is Kipnis’ extrapolations of the implications of this research. His research team has not conducted any studies into what these results mean for any neurological disorders nor has he drawn on any previous studies that could lend credence to his claims. To put it simply, this is just bad science.
Banks, W. A. (2015). The blood-brain barrier in neuroimmunology: Tales of separation and assimilation. Brain, Behavior, And Immunity, 441-8.
Louveau, A., Smirnov, I., Keyes, T. J., Eccles, J. D., Rouhani, S. J., Peske, J. D., & … Kipnis, J. (2015). Structural and functional features of central nervous system lymphatic vessels. Nature, 523(7560), 337.
I’m guessing Kipnis et al wanted their paper to go out as soon as possible to avoid being scooped. That’s probably why they quickly published without doing more studies to determine what the implications are behind this finding. I wouldn’t blame them just yet. They did manage to get a publication in Nature, and I’m sure that there are ongoing studies to see what’s going on in the lymphatic system in the CNS. And studying mouse brains is obviously easier than studying human brains.
Others have spent a lot of time trying to elucidate the mechanisms by which the central nervous system transports its lymphocytes and moves interstitial fluid from tissues. Small molecules pass through the blood brain barrier relatively easily. But, how do large molecules move through? And how might lymphocytes travel to the CNS? Due to the difficulties in studying the human brain, we likely have a lot of work to do before we have satisfactory answers to these questions.
Source:
Iliff JJ, Nedergaard M. Is there a Cerebral Lymphatic System? Stroke. 2013 Jun: 44(6 0 1): S93-S95.
Bad science? He has clearly shown that there are lymphatic vessels in the brain of mice, and the study has been published in one of the very top scientific journals. Not doing studies related to neurological disorders does not make it bad science.
The research paper was complete and was answering a specific research question. It adds considerably to our understanding of neuroimmunology — it’s a fantastic novel, clear finding that will spearhead additional studies looking at neurological disorders.
Maybe you should revise your views of what is good and bad science.
Furthermore, please consult the paper that was published in October of this year, which another reader of this post, Ezinne Eneh, talked about. This is a review paper that shows that the presence of lymphatic vessels of the dura mater has been found in a few other older studies in humans.
You both seem to be under the impression that anything published in a journal as reputable as Nature is beyond all reproach and should be taken as absolute. In reality everything, even those studies in Nature, should be looked at with a critical eye. I can think of two studies just off the top of my head that are prime examples of this very thing. The first being the infamous Wakefield paper published in the Lancet (another very reputable journal) and the second two papers conducted by Hwang Woo-Suk published by Science (a journal equal to that of Nature). Arguing that something must be true because it has managed to be published in Nature is not pertinent to the validity of the study actually being presented.
That being said, however, I’m not discounting the results of this study. Just erring on the side of caution until further research can be done, perhaps in other animal models and/or humans. When I said the researcher was acting in bad science I was not referring to the actual study itself but rather Kipnis’ claims in his press release of the higher implications of this research in neurological disorders. So far as I can tell there is no evidence to support this claim and could even potentially be damaging to his own career and reputation if this turns out to be unfounded. Not only does this sort of grandiose posturing harm the claimant but it also in turn hurts science.
Hwang WS, et al. (2004). “Evidence of a pluripotent human embryonic stem cell line derived from a cloned blastocyst”. Science 303 (5664): 1669–74.
Hwang WS, et al. (2005). “Patient-specific embryonic stem cells derived from human SCNT blastocysts”. Science 308 (5729): 1777–83.
Wakefield AJ; Murch SH; Anthony A; et al. (28 February 1998). “Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children”. Lancet 351 (9103): 637–41
I completely understand where you are coming from, M. Creech. I am often in the habit of taking every paper I read, even ones that come from such a prestigious journal such as Nature, with a grain of salt. It is not because I believe that there are any blatant errors or efforts to mislead, but because science is often disproven as time passes. A piece of knowledge that used to be taken as the gospel truth (that the CNS had no lymphatic system) was shown to be incorrect. In time there will most certainly be papers that elucidate the exact significance that this discovery has upon the understanding of various diseases. However, I don’t think that this scientist would put his career on the line by making wild guesses as to where this discovery could lead.
More often than not when a researcher talks about implications or future directions based on a current discovery, they do so comfortably because they have either given it a good deal of thought and the physiological mechanisms for which this could be true seem logical, or because they have already started pilot studies using various models of disease and they have returned some promising initial findings. That is, after all, how a lot of science gets funded: you take logical, educated guesses upon an outcome and use it as a working hypothesis while having a general idea as to where your data is going to lead you. If they talked about the need to reconsider Alzheimer’s and MS as an immune disease it is more likely than not because they have some sort of data that points them in that direction.
Indeed no one has ever found any lymphatic vessel in human Meninges, because the key method they use in their discovery is fixing the mice meninges tissue under physiological stage before running any test. I personally assume that this “physiological stage” here suggests that the mice meninges tissue is extracted by vivisection or by injecting fixing solution to living mice brain. If this is the only possible way to detect lymphatic vessel in meninges, it’s quite hard to imaging similar operation on human.
I wouldn’t be surprised if the lymphatic vessels did not exist in the CNS in humans. After all of the surgeries and dissections we have done on humans, no one has noticed lymphatic vessels in the CNS, then I do not believe they exist. However, as Antoine Louveau states, they may have not been discovered due to their unique complex locations. But I’m sure there have been surgeries on humans on every part of the body, at least dissections by pathologists or medical students. If they do exist in humans, I’m surprised they have not found it yet. It would be interesting to see if our closest ancestors, the chimpanzees have lymphatic vessels in their CNS. After a search on pubmed, I found this article by Bucchieri et al., 2015 but I do not have free access to it so I cannot see anything except for the key words, no abstract. This was published this month, so perhaps this article sheds light on Lymphatic vessels in the dura mater. Another article by Aspelund A et al., 2015 describes the anatomy of the lymphatic vessels of the mouse brain as well. It seems as though researchers sure are looking into this, but will take time.
I have done a lot of research on Multiple Sclerosis in my previous graduate degree thesis and this is very interesting for me. If true this could shed new light into other autoimmune and neurologic diseases. If it is true that certain neurologic diseases such as Alzheimer’s can be caused from a backup of proteins in the brain not being filtered by the lymphatic vessels in the CNS, then this could lead to revolutionary findings and treatments for these diseases. Perhaps Kipnis is hyping up their research a bit too much? If, in cases of inflammation in patients with MS, Alzheimer’s, or other neurologic diseases that show inflammation in the CNS, wouldn’t MRI’s show possible lymphatic vessels that were inflamed or blocked? I think we would have seen imaging proof, if these vessels do exist in humans.
As Trisha noted, we should take this with a grain of salt, since there is no hard evidence for lymphatic vessels in the CNS in humans. Should we focus more on imaging techniques or on dissections? Perhaps we start with Chimp dissections of the meninges and dura, and perhaps human cadavers. Hopefully the next year or two there will be further research coming out to shed light on the existence or lack of existence of lymphatic vessels in the CNS in humans.
References
Aspelund, A., Antila, S., Proulx, S. T., Karlsen, T. V., Karaman, S., Detmar, M., . . . Alitalo, K. (2015). A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. The Journal of Experimental Medicine, 212(7), 991-999. doi:10.1084/jem.20142290 [doi]
Bucchieri, F., Farina, F., Zummo, G., & Cappello, F. (2015). Lymphatic vessels of the dura mater: A new discovery? Journal of Anatomy, 227(5), 702-703. doi:10.1111/joa.12381 [doi]
Louveau, A., Smirnov, I., Keyes, T. J., Eccles, J. D., Rouhani, S. J., Peske, J. D., . . . Kipnis, J. (2015). Structural and functional features of central nervous system lymphatic vessels. Nature, 523(7560), 337-341. doi:10.1038/nature14432 [doi]
I find this research very thought provoking. As a neuroscience student and anatomy teacher, I’ve always thought about how the blood brain barrier purposely isolates the CNS. This network of cells and capillaries is very selective of what kinds of molecules can enter the chemical environment of the brain and for good reason – the CNS is responsible for controlling and regulating body functions and how we respond to our environment. I am actually surprised to find that there is quite a bit of research surrounding the topic of how the immune system functions with and around the blood brain barrier; a quick search results in numerous scholarly articles
The fact that we are seeing lymphatic vessels in the meninges of any species means that there is a way for cells that mature in the secondary lymphoid organs to get to the brain or at the very least the tissues and fluid that surround the brain. My question is if there is a way for immune cells to enter via lymphatic vessels, how did the pathogens that are making this necessary get there in the first place? If the blood brain barrier is as exclusive as previously thought then it doesn’t make sense to think that many antigens would be able to access this exclusive anatomical real estate. A previous commenter is correct that human tissue has yet to be investigated but as is the case with many, many other scientific questions, obtaining human subjects for testing is problematic at best. It will be interesting to see where this research leads, especially given how many neurological disorders still have no known cause or the cause is poorly understood.
http://www.sciencedirect.com/science/article/pii/S0969996109002095
http://journals.lww.com/jneuropath/Abstract/2003/06000/The_Blood_Brain_Barrier_and_Its_Role_in_Immune.1.aspx
http://www.sciencedirect.com/science/article/pii/S1545534306700189
http://www.jleukbio.org/content/72/6/1075.long
The nervous system is the most complex and least understood organ system of them all. It is known that the Nervous system and the Immune system communicate with each other, given the presence of immune cells defending against organisms and fluid containing soluble immune mediators in the brain and spinal cord. Originally, there was no evidence lymphatic vessels were present in the central nervous system. Therefore, researchers were unsure how these cells were able to cross the barrier, since the blood brain barrier is highly impermeable. However, after further investigation, it was revealed that immune cells and fluid are produced by deep cervical lymph nodes. Given these findings, I think it is important to investigate the correlation between certain nervous system diseases such as multiple sclerosis and Alzheimer’s to identify if there is any lymph vessel damage associated with these diseases. I am sure lymph vessel damages occur with age, but I would also want to identify environmental and social factors that could be associated with increase damage to these blood vessels. For example, I would want to identify if alcohol or smoking promotes further damage of the lymphatic vessels.
I find it interesting that the article presents the findings of the University of Virginia School of Medicine researchers as though they were new. In reality, there have been previous findings of lymphatic vessels in the CNS, not just in animal models, but they do exist in humans as well. One of the earliest findings was in 1978 when Mascgagni observed the presence of lymphatic vessels in human dura mater. In 1953 and 1196, Lecco and Li et al respectively, also observed the presence of lymphatic vessels in human dura mater. [1] One of researchers from the University of Virginia School of Medicine, Kipnis, noted that the vessels were “very well hidden”. This is in line with the findings of Lecco in 1953 because he was able to find lymphatic structures in only 4 out of the 30 human subjects that he examined. [1] Although he believed that that result indicated that the dura mater of these subjects developed differently for different functional reasons, I believe that the difficulty in finding the lymphatic vessels in the CNS is a better indication. The difficulty of finding these lymphatic vessels may shed light to why outcomes of researchers successfully identifying them in the CNS appear sparse. The proper identification of lymphatic vessels involved with neurogological disorders that affect the immune system may improve our understanding of their pathology and improve diagnostic as well as treatment models.
Citation
Bucchieri F., F. Farina, G. Zummo and F. Cappello. Lymphatic vessels of the dura mater: a new discovery? Journal of Anatomy. 227: 702-703.
website link: http://onlinelibrary.wiley.com/doi/10.1111/joa.12381/full
Ezinne, I think you meant 1787 with respect to Mascagni . Paolo Mascagni was a professor of anatomy at the University of Siena, Italy in the late 1700’s, who expanded on the discovery of lymphatics in the head and neck through a mercury injection technique (1). Mascagni’s findings did not suggest that the lymphatics were part of the CNS, and his iconic drawings depict the lymphatic vessels in the dura mater – not a component of the neuraxis, but its covering. Subsequent researchers identified extensive lymphatic networks in the superficial tissues of the head and neck and the dermis, using a variety of different visualizing techniques, but all external to the CNS (Id). The authors of the article in the Journal of Anatomy that addressed the recent research finding lymphatic vessels in the human brain specifically noted that a) this is not a “new” discovery, citing Mascagni and additional studies dating back to 1953; b), that the lymphatic vessels identified are not “in” the brain, but in the meningeal covering of the brain and spinal cord; c) the vessels that were found in only 4 of 30 human brain meninges were felt to have been the result of a functional development; and d) when present, dural lymphatics can absorb CSF, and lymphatic cells may migrate through the ependymal layer to the CSF and into the lymphatics, as part of the blood-brain barrier. It is the blood-brain barrier, which prevents the formation of interstitial fluid in the nervous tissue, that Bucchieri et. al. emphasize as the reason why it is not necessary to have lymphatic tissue within the CNS (2).
I cannot agree with the conclusion that the structures Kipnis found were “hidden” in the human brains in all of the other research instances where they were simply not identified. Kipnis’ statement referred to the infrequency with which he found the structures in mouse brains, and absent evidence, should not be automatically extrapolated to humans. I agree with Bucchieri et. al. that, in all likelihood, their development occurs under specific conditions, in response to specific events, but still does not automatically mean that there is “hidden” lymphatic tissue within the CNS. I look forward to future research.
1. Pan, W.; Wang, D. 2013. Historical review of lymphatic studies in the head and neck. Journal of Lymphoedema (Online), 8 (1), 43-46. http://www.journaloflymphoedema.com/media/issues/920/files/content_11242.pdf (accessed 12/5/15).
2. Bucchieri, F.; Farina, F.; Zummo, G.; Cappello, F. 2015. Lymphatic vessels of the dura mater: a new discovery? Journal of Anatomy (Online), 227 (5), 702-703. http://Onlinelibrary.wiley.com/doi/10.1111/joa.12381/full (accessed 12/5/15).
I find it interesting how the scientific community is disproved time and time again on their initial hypotheses and theories. Lymphatic vessels were first thought to not exist within the CNS, however recent studies seem to suggest that they may have been in humans the entire time. An experiment revealed that a mouse’s meninges possessed lymphatic vessels that albeit were very hard to observe and concealed in a way that was previously undetectable. Critically, if these vessels are found to also be in humans it could explain the root cause of neurological degeneration. These vessels are very important for the transport of immune cells and also the activation of lymphocytes. It is very possible that a breakdown of these vessels could lead to major immunologic effects leading to disease. Confirmation of the presence of these vessels in humans now becomes the main concern at hand. If found, methods of detecting and preventing protein accumulation in these vessels may be the key to solving neurological diseases.
Multiple sclerosis is a common neurological disorder that is caused and effected by immune system related mechanisms and their interaction with the CNS. This form of autoimmunity may be further explained by the function of these newly discovered lymphatic vessels if they are indeed found in humans. Malfunctioning vessels could significantly contribute to the rate at which MS can utilize the immune system to destroy nerves in the brain.
Patejdl, R., Penner, I., Noack, T., & Zettl, U. (2015). Multiple sclerosis and fatigue: A review on the contribution of inflammation and immune-mediated neurodegeneration. Autoimmunity Reviews. doi:10.1016/j.autrev.2015.11.005
I find it quite intriguing that new findings have shown that there are, in fact, lymphatic vessels connecting the CNS to the deep cervical lymph nodes. As explained, this is an easy to miss anatomical characterization, now found in mice. However, the question is, is this the same make-up that is present in humans. Agreeably, I think that this is very likely a characteristic of humans as well and further research will solve the mysteries by linking immunological malfunctions for in patients with neurological disorders. As previously found in preclinical and clinical studies, that immune-mediated actions contribute to and drive Alzheimer’s disease (AD) pathogenesis (Heppner, 2015). Understanding that inflammation and microglial (predominant macrophage species within the brain) activation are central characteristics of Alzheimer’s disease (Schott, 2013) and that the immune response involved in the disease is the innate immune response should definitely set off research missiles. The inflammation is the signaling cause that leads to neuronal and synaptic damage (Schott, 2013). These simple understandings are alarming facts that should tell the story that there has to be a direct connection of the CNS to the immune system. AD is a good model for studying the immune system-central nervous system relationship.
Scientist could develop novel therapies on the basis of inflammation and a better understanding of the exact immune cells involved in the disease. Although some anti-inflammatory medications have shown no significant effect on the disease, it is still very necessary for future studies focusing on the key responders involved in the neurological disease. The Kipnis laboratory is off to a good start, as they stated, the vessels could easily be missed if it is not clear exactly what you are looking for. It could have easily been missed, mistaking the vessels as part of the blood vessels that they are close to. I would like to see the meninges from human brains histologically / pathologically studied to prove that we are in fact running off of this same mechanism as seen in the mice.
Works Cited
Heppner, F. R. (2015). Immune attack: the role of inflammation in Alzheimer disease . Nature Reviews Neuroscience , 16, 358-372
.
Schott, J. a. (2013). Inflammation in Alzheimer’s disease: insights from immunotherapy. Journal of Neurology .
I found it a good example of research where we disapprove something which has been approved previously. Nothing is wrong in this because it shows the improvement in research with time. Human have closed type of circulatory system unlike open type which is found in lower living organisms. According to a research central nervous system lack classical lymphatic vessels but the the immune surveillance occur in meningeal compartment. The mechanism behind the entry and exit of immune cells were unknown. Immune responses in the CNS are common, despite its perception as a site of immune privilege. These responses can be mediated by resident microglia and astrocytes, which are innate immune cells without direct counterparts in the periphery.
DCs play a critical role in activation and initiation of T cell responses by taking up protein antigens in tissues, breaking them into small peptides and then displaying them on their surface physically associated with MHC class II molecules. DCs migrate through afferent lymphatics to draining lymph nodes and present antigen to naive or memory T cells. Importantly, there is no evidence that DCs with such capacities reside in the healthy CNS parenchyma, nor do CNS resident immune cells prime naive T cells. Microglia, the resident immune cells of the central nervous system (CNS), play an important role in CNS homeostasis during development, adulthood and ageing.
References:
Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, Derecki NC,
Castle D, Mandell JW, Lee KS, Harris TH, Kipnis J. Structural and functional
features of central nervous system lymphatic vessels. Nature. 2015 Jul 16
Weller RO, Engelhardt B, Phillips MJ. Lymphocyte targeting of the central
nervous system: a review of afferent and efferent CNS-immune pathways. Brain
Pathol. 1996 Jul;6
Kiwic G, Slusarczyk K, Slusarczyk R. [The central nervous system and the
lymphatic system. Lymphatic drainage of the cerebrospinal fluid]. Neurol
Neurochir Pol. 1998 May-Jun
I always wonder about the anatomical and physiological status of sinuses in the human skull. Why do they need to be there? Scientists are not sure about their physiological significance. Although most probable rationalization of their anatomic location is that sinuses make our skull lighter and physiologically make us sound better by helping in sound resonance. Later research came out with findings of their immunological intervention too. But as stated in this recent research about the location of central lymphatics, so it intrigues me with an idea that sinuses in our skull may be an easy way out for central lymphatics. It can be possible as they are located quite near to tonsils and other secondary lymphoid organs such as deep cervical lymph nodes. Once the status of the central lymphatic system is established, then it will explore new perspectives on the existence of sinuses.
Reference: doi:10.1038/nature14432
I never thought about the sinuses in the human skull this way. I’ve always read and heard that the brain’s ventricles and CSF flow contribute to reducing the weight of the skull. When people have a blockage of their ventricular system, CSF build-up can be hard to identify. The build-up of CSF in the brain has been linked to a reduction in overall weight. I think the sinuses may be similar in terms of an immunological role in that they are used to filter microbes and allergens out of the body. Some studies on the maxillary sinus have suggested that it is necessary for growth of facial structures because it is easier to have growth around cavities. It also seems to play a role in the transmission of shockwaves during traumas.
Dargaud J, Cotton F, Buttin R, Morin A. The maxillary sinus: evolution and function in aging. Morphologie. 2003;87(276):17–22
The bones of the face and skull contain air-filled pockets called sinuses. Every single sinus has an opening that connects the sinus to the nose. This opening is called an ostium. Except for the two frontal sinus that we have, each sinus develops from a very tiny pea-sized pocket, during childhood, to a bigger walnut sized-structure. The main function of sinuses is to produce mucous. The mucous that is produced by the sinuses moisturize the internal portion of the nose. The accumulation of mucous forms a layer. This layer protects the body from pollutants, microorganisms, dust and dirt that may enter through the nose. The nose consists of tiny hair cells called cilia. These hair cells have the ability to move the mucous backwards slowly until it is finally in the throat and then ingested. The sinuses actually function as an immune component by protecting the body against air-borne pathogens that may be eliminated through the sinuses.
(http://www.cedars-sinai.edu/Patients/Programs-and-Services/Sinus-Center/Anatomy-of-the-Sinuses.aspx)
One thing that most struck me about the research carried out by doctors Westermann and Lange, was the observation that the down-regulation of cholinergic activity is one of the factors that contributes to facilitating the presentation of antigens and therefore commitment of information gathered during the innate to long term adaptive memory. The role of the cholinergic pathway itself capable of directly acting upon the immune system through the vagus nerve which through release of acetylcholine. In other tissue, such as smooth muscle acetylcholine may induce action. However, activation of the Nicotinic acetylcholine receptor α7 expressed in macrophages and Lymphocytes instead induces a sort of anergy through signal transduction that amongst their end results include the down regulation of TNF and other inflammatory cytokine release.
This interaction between the CNS and humoral immune system has been referred to as Neuroimmunomodulation. Through receiving immune signals through the vagus nerve or humor, the CNS is capable of receiving information on the body’s inflammatory state. The CNS in turn can effect change on the body’s inflammatory state though both inducing the release of steroids and acetylcholine release through the vagus nerve. In a healthy subject, this functions as a means for controlling excessive inflammation however prolonged Cholinergic Anti-inflammatory signals have the potential to interfere with the activities needed to produce an acquired immune response. The ability of sleep to temporarily suppress Cholinergic, therefore, allows a window for unimpeded presentation and response to take place. This interaction between CNS and Immune is a potential target for various therapeutic applications. While sleep may be useful for antigen presentation, upregulation of the Cholinergic Anti-inflammatory Pathway through cholinergic drugs may be a viable way to suppress chronic inflammation.
Thus, the Nicotinic acetylcholine receptors in leukocytes and the nervous system, both paralogues conserved from the signaling mechanisms found in primitive ancestors, present a bridge between both worlds. Therapeutic manipulation of Neuroimmunomodulation may present a new avenue for treating conditions caused by immune dysregulation.
Bibliography: 1. Valentin A Pavlov K. The Cholinergic Anti-inflammatory Pathway: A Missing Link in Neuroimmunomodulation. Molecular Medicine. 2003;9(5-8):125. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1430829/#!po=1.19048. Accessed November 29, 2015.
Bibliography: 2. McAllen R, Cook A, Khiew H, Martelli D, Hamilton J. The interface between cholinergic pathways and the immune system and its relevance to arthritis. Arthritis Res Ther. 2015;17(1). doi:10.1186/s13075-015-0597-2.
Bibliography: 3. Razani-Boroujerdi S, Boyd R, Davila-Garcia M et al. T Cells Express 7-Nicotinic Acetylcholine Receptor Subunits That Require a Functional TCR and Leukocyte-Specific Protein
Tyrosine Kinase for Nicotine-Induced Ca2+ Response. The Journal of Immunology. 2007;179(5):2889-2898. doi:10.4049/jimmunol.179.5.2889.
The central nervous system and the immune system need to have communication to relay information to the rest of the body. The question here is does the immune system use lymphatic vessels to exchange immune cells with brain tissue or not. Antoine Louveau proved that there were lymphatic vessels and were problem missed before because they might have been hidden. My thoughts are it would only make sense that there were lymphatic vessels because what happens to the bacteria/parasites that travel to the brain. The body has to try and fight off these infections some how especially that there isn’t a direct path for leucocytes to travel to the brain. Of course, there is the blood-CSF barrier that consists of epithelial cells to maintain the central nervous system homeostasis by producing cerebrospinal fluid (CSF) to restrict pathogens entering the brain. If this blood brain barrier is disrupted then we can find ourselves in multiple issues. Either a pathogen can find its way to the brain or macrophages can invade the brain.
Because the lymphatic vessels were very hard to identify, scientist went about finding other ways to understand the body. The role of cervical lymph nodes in T cell mediated immune reactions in the brain was studied and saw that the regional lymph nodes play a major role in T and B cell mediated immune reactions of the CNS. They also have a major role in the induction of tolerance to CNS proteins and neuro-immunological responses. Studies have also shown lymphatic drainage of ISF along perivascular pathways to cervical lymph nodes and drainage of CSF to nasal lymphatic that sub-serve immunological responses in the CNS. If the lymphatic drainage of the CNS as well as the newly identified lymphatic vessels is further studied then therapeutic approaches for huge diseases such as MS can be resolved.
Weller, R., Galea, I., Carare, R., & Minagar, A. (2010). Review: Pathophysiology of the lymphatic drainage of the central nervous system: Implications for pathogenesis and therapy of multiple sclerosis. Pathophysiology, 17(Lymphatic Vessel Functions in Health and Disease), 295-306. doi:10.1016/j.pathophys.2009.10.007
One topic most people learn about in Immunology is the blood brain barrier (BBB) and its impermeability. That impermeability is the sole mechanism the brain has to fight infection, by not letting pathogens in to begin with. But this study confirms the BBB gets a little help from the lymphatic system. A study published in ImmunolRev highlights antibodies as the mediators of brain pathology in lupus patients. It states that antibodies only enter the brain when the BBB is compromised. The study focuses on the autoimmune disease lupus and how it auto anti-brain antibodies lead to neurological pathology. However, it would be interesting to see research that shows, if anything, how the lymphatic system in the brain could attribute to the access of anti-brain auto antibodies found in lupus patients.
Works Cited:
ImmunolRev. 2012 Jul: 248 (1) 56-67.
Because of the blood-brain barrier allowing only a little few of components transported into the brain and prevent the brain from being damaged by multiple infection and toxins, it’s reasonable to infer that the function of the immune system in the brain is mainly focusing on maintaining homeostasis and tissue renewal. However, the discovery of the lymphatic vessels provides new possibility in the path of pathogens getting into the brain. The design of their experiment is brilliant, for they managed to fix the mice meninges tissue under physiological stage and run a whole detecting. It’s easy to conduct but the idea is hard to come up with.
Making conclusions without thorough research is an unsafe practice because of the future misleads it can create. This has been the case in the conclusion that “Lymphatic vessels are not found in CNS tissues”. One would naturally think that there’s some sought of protection for the brain and spinal cord besides the cerebrospinal fluid; especially immune related. Dr. Louveau’s initiative to further study Lymphatic vessels and CNS tissues should be applauded. His discovery is groundbreaking because it sheds new light on diseases such as multiple sclerosis and Alzheimer’s disease. Further research with Dr. Louveau’s finding will bring potential new drugs against CNS related disease in the future.
Dr. Louveau’s findings happens to be in mice and poses the question; “Do CNS Lymphatic Vessels exist in humans?” Communication is everything. There has to be a means through which CNS tissues communicates with the cerebrospinal fluid to get rid of waste. The cerebrospinal fluid is also known to have connections with the lymphatic system. Based on this, I believe Lymphatic vessels exist in humans.