Type 2 inflammatory responses involve both innate and adaptive immune systems and are triggered by exposure to infectious pathogens and environmental antigens, as for example helminths, allergens, and venoms. These responses are characterized by activation of T helper 2 cells and subsequent release of type 2 cytokines, such as interleukin-4 (IL-4), IL-5, IL-9, and IL-13, resulting in production of immunoglobulin E (IgE) and activation of different types of effector cells—basophils, mast cells, and eosinophils. Typically, these responses promote increased mucus production and muscle contractions which, together, help to expel the parasite or allergen from the body.
Group 2 innate lymphoid cells (or ILC2s for short) are a potent source of type 2 cytokines and therefore are involved in type 2 inflammatory responses. These cells are present in human lung tissue, peripheral blood, gastrointestinal tract, skin, and sinonasal tissue, and likely contribute to chronic rhinosinusitis, asthma, atopic dermatitis, and gastrointestinal allergic disease.
Results from a study published in the scientific journal Science (2-adrenergic receptor–mediated negative regulation of group 2 innate lymphoid cell responses) show that ILC2s are involved in a crosstalk between the nervous and the immune system, thus playing an important role in regulating acute and chronic inflammation. But what are the mechanisms at the basis of these regulatory processes?
Researchers used mice to discover that ILC2s express the β2-adrenergic receptor (β2AR) and are located in the intestine in close proximity to adrenergic neurons. Adrenergic neurons release either the neurotransmitter adrenaline (epinephrine), or noradrenaline, or dopamine, which interact with β2ARs—β2ARs give nerve cells the ability to interact with each other and influence the immune response.
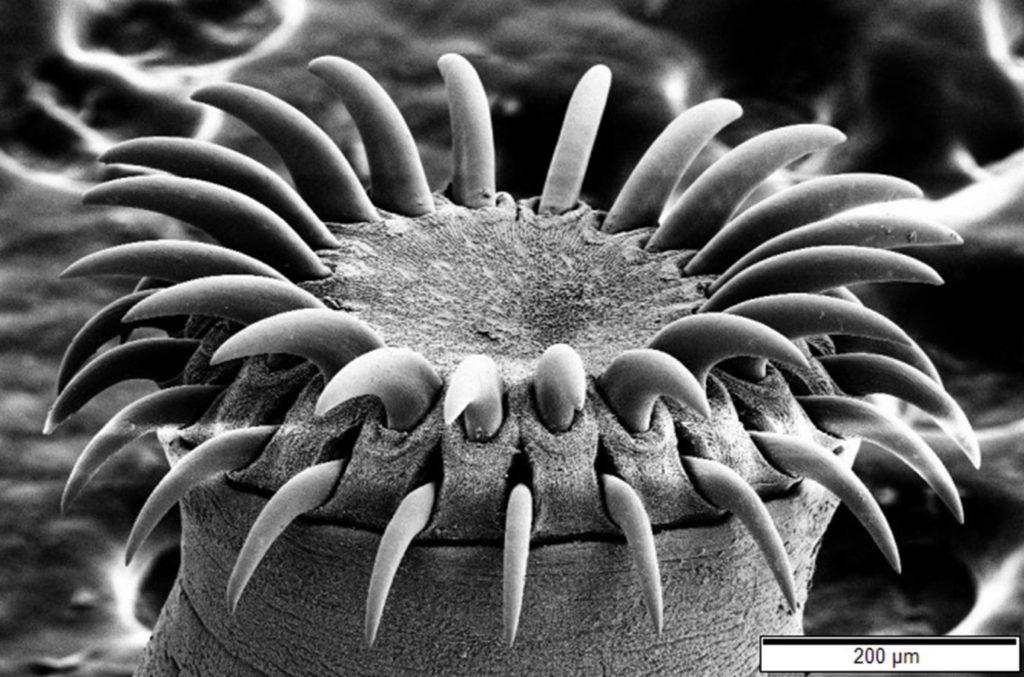
The researchers then infected mice that lack β2ARs with the gastrointestinal helminth Nippostrongylus brasiliensis, which was already known to induce potent ILC2 responses that play an important role in the expulsion of the parasite through production of IL-5 and IL-13. These mice had exaggerated ILC2 responses to the helminth infection in intestinal and lung tissues resulting in faster expulsion of the parasites. By contrast, when they treated normal mice with drugs that stimulate β2AR, the immune response was blunted and the helminth infections worsened. In addition, the researchers found that the β2AR pathway negatively regulates the ILC2 responses through inhibition of cell proliferation and effector functions. Collectively, these data provide the first evidence of a neuronal-derived regulatory circuit that limits ILC2-dependent type 2 inflammation. All together, the study results highlight a previously unrecognized regulatory circuit that operates between the adrenergic nervous system and the innate immune system to control type 2 inflammation at multiple mucosal sites.
The most commonly used drugs to treat asthma also stimulate β2AR, which may explain why they are so effective at controlling allergy symptoms. David Artis, senior author of the study, said in a press release: “We must have given tens of millions of doses of these drugs to shut down the acute symptoms of asthma. Nobody could agree on how these drugs work, but it may be that they are working in part through targeting the innate immune system. If we understand more mechanistically how this class of drugs works, it might give us new avenues to develop additional therapies built around the biology.”
In their published paper, the researchers conclude that the mammalian nervous system appears to have evolved dual mechanisms to rapidly activate or repress group 2 innate lymphoid cells to protect the host against diverse inflammatory stimuli.




As mentioned in the blogpost, Innate lymphoid cells or ILCs are involved in a cross talk with the immune system and the nervous system. Upon research, an article titled Innate Lymphoid Cells: A Link between the Nervous System and Microbiota in Intestinal Networks further described the relationship between the Enteric Nervous System (ENS) and ILCs. The ENS is referred to as the intestinal brain and consists of myenteric nerve plexuses and submucosal plexuses along with exogenous neurons that affect immune responses (Han et al., 2019). The article stated that although a relationship between ILCs and the ENS are still unclear, studies have shown that the ENS activates ILCs. The ILCs then release cytokines. The article further refers to the ENS as a surveillance monitor for the immune system because ILCs receive instructions from the nerve cells. Similar to the blogpost, a study on the ILC2s of mice was observed. The results from the study were that neurons secrete neuronal messenger U (NMU) that activated ILC2s, and created a rapid immune response (Han et al., 2019). Studying the human body’s ILC interactions would help gain more insight about the connection between the nervous system, immune system, and ILCs than the knowledge that is present today.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6360575/
Han, L., Wang, X. M., Di, S., Gao, Z. Z., Li, Q. W., Wu, H. R., Wang, Q., Zhao, L. H., & Tong, X. L. (2019). Innate Lymphoid Cells: A Link between the Nervous System and Microbiota in Intestinal Networks. Mediators of inflammation, 2019, 1978094. https://doi.org/10.1155/2019/1978094
This post offered an in depth look into one of the interactions between immune and nervous systems. Group 2 innate lymphoid cells are involved in a previously unknown regulatory circuit connecting the adrenergic nervous system and the immune system. I found an article, “Regulatory Innate Lymphoid Cells Control Innate Intestinal Inflammation”, that tries to find a better understanding of how intestinal inflammation is impacted by ILCs. This study focused on a subgroup of ILCs called ILCregs that inhibit the gut and contain unique genes from other ILCs. When inflammation is stimulated here, ILCregs in the gut can be induced to suppress ILC1s and ILC3s. This suppression occurs because of IL-10 secretion which protects against innate intestinal inflammation.
Refernce: Wang, Shuo, et al. “Regulatory Innate Lymphoid Cells Control Innate Intestinal Inflammation.” Cell.com, http://www.cell.com/cell/fulltext/S0092-8674(17)30863-2?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0092867417308632%3Fshowall%3Dtrue.
Hello, Cray!
Innate lymphoid cells (ILCs) are activated and secreted by cytokines that maintain homeostasis and fight infection in the gut. Before reading this blog post, I was not aware of ILCs many derivatives and their production. Your comment encouraged me to research derivative IL-10 and ILCreg; I found the article ILC2s are the predominant source of intestinal ILC-derived IL-10 by Bando, JK et al.
Protozoa and parasitic helminths induce ILC2s (group 2 of innate lymphoid cells) production of IL-10. IL-10 supports homeostasis in the intestines. Researchers, Bando JK et al., discovered ILC2s provide a source of IL-10 in the gastrointestinal tract and ability to suppress T reg cells cytokine production of ILC2s and ILC3’s in the intestine, confirming your article’s theory.
Two follow up studies were conducted with Lin−CD45+CD127+, small and large intestine lymphocytes cells. The first experiment analyzed natural killer cell markers in the small intestine, showing Lin−CD45+CD127+ cells lacked ILC2 and ILC3 markers, but instead GATA3hi ILC2s or RORγt+ ILC3s. During an eight-day experiment, a DSS-induced injury and infection to test intestinal inflammation by giving 3% DSS in mice drinking water. On day eight, there was no increase of ILC1-3s population, alluding that ILCregs may not affect ILC2-3s suppression.
Reference:
https://www.ncbi.nlm.nih.gov/pubmed/31699824
After reading this blog post, I was interested in learning more about the role ILC2s had in treating asthma patients. Previous studies have confirmed that there is an association with ILC2s and asthma as it is responsible for mediating asthmatic inflammation. A study conducted by Yu et. al, was aimed at evaluating ILC2 activity in asthma patients after undergoing glucocorticoid therapy. It was determined that following the administration of glucocorticoids for three months in patients with both asthma and allergic rhinitis, the circulating levels of ILC2 along with IL-5, IL-13, and IL-9 decreased at one and three months after the treatment. Thus, using glucocorticoids could be an effective means to treat asthma by regulating the circulating levels of ILC2 and reducing the inflammatory response to allergens.
Reference:
Yu, QN, Guo, YB, Li, X, et al. ILC2 frequency and activity are inhibited by glucocorticoid treatment via STAT pathway in patients with asthma. Allergy. 2018; 73: 1860– 1870. https://doi.org/10.1111/all.13438
Upon reading the article and your comment I ran across this article, which kind of explained how the B2ARs help control the state of the acute disease. Like ILC2, which help in mediating asthmatic inflammation, these B2ARs follow the same concept, these beta-agonists provide mediation in the same criteria. The study done on mice induced with asthma, using B-agonists showed immense results of the reduction of the acute disease within the mice. The use of the chronic treatment with therapeutic b-agonists, through activation of B2AR-mediated signal pathway, promoted in the severity of asthma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3085865/
Upon reading this article I was curious to learn how B2AR is stimulated by drugs and helps asthma patients. It also arose my curiosity on how B2AR could treat asthma patients. The B2-adrenoceptor is known as the most studied proteins in biology, B2AR is considered a protypical GPCR according to the article “New perspectives regarding B2-adrenoceptor ligands in treatment of asthma” asthma represents restricted airflow, B2AR-agonists, which are used to reverse acute bronchoconstriction by inhaling the receptor via a inhaler. The agonist acts on the airway of smooth muscle cells B2Ars to counteract the procontractile agents and then help relax the airways. However, the response to these beta-agonists does vary on different patients. The article states that B2ARs play a huge role in asthma pathogenesis and their therapeutic effectiveness when you are inhaling these beta-agonist. Beta-agonists against asthma have a strong therapeutic tendency, and control the state for a long time.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3085865/
Walker, J. K., Penn, R. B., Hanania, N. A., Dickey, B. F., & Bond, R. A. (2011). New perspectives regarding β(2) -adrenoceptor ligands in the treatment of asthma. British journal of pharmacology, 163(1), 18–28. https://doi.org/10.1111/j.1476-5381.2010.01178.x
ILC2s are involved in a crosstalk between the nervous and the immune system, thus playing an important role in regulating acute and chronic inflammation.
ILC2s express the β2-adrenergic receptor (β2AR) and are located in the intestine in close proximity to adrenergic neurons.
β2AR pathway negatively regulates the ILC2 responses through inhibition of cell proliferation and effector functions.
neuronal-derived regulatory circuit that limits ILC2-dependent type 2 inflammation
The most commonly used drugs to treat asthma also stimulate β2AR, which may explain why they are so effective at controlling allergy symptoms.
the researchers conclude that the mammalian nervous system appears to have evolved dual mechanisms to rapidly activate or repress group 2 innate lymphoid cells to protect the host against diverse inflammatory stimuli
The blog post above mentions that ILC2s express the B2-adrenergic receptor and are found in the intestine close to adrenergic neurons, these neurons release neurotransmitters that interact with the B2-adrengergic receptor and influence the immune response during infection. Ultimately, they found that when mice were infected with a gastrointestinal pathogen and lacked the B2-adrenergic receptor, they had a more exaggerated immune response to the infection in the intestines and lungs which got rid of the parasite quicker. When mice with the B2-adrenergic receptor were infected, they had a weaker immune response which caused the infection to get worse. Thus, they were able to conclude that stimulating the B2-adrenergic receptor on the ILC2s inhibited effector function and cell proliferation. Neural stimulation of the B2-adernergic receptor negatively regulated ILC2-dependent type 2 inflammation. This provides evidence that the nervous system is linked to the immune response via these ILC2s. But the blog post described how it was negatively regulated. I wanted to know if the nervous system was involved in activating ILC2s in orchestrating a strong immune response and if there is another way another way neurons and the nervous system communicated with these ILC2s in the gastrointestinal tract during helminth infection other than via neurotransmitters and the B2-adrenergic receptor. I found this article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6066372/ where they report that ILC2s are the only hematopoietic cells that express the NMU receptor 1 which binds to the neuropeptide neuromedin U (NMU) on cholinergic neurons in the gastrointestinal tract which allows the two cells to co-localize. When the ILC2s were stimulated by NMU in vivo, the cells were rapidly activated, proliferated, and secreted type 2 cytokines IL-5, IL-9, and IL-13. When the cells were administered NMU in vivo, the ILC2s were activated and proliferated and they recruited eosinophils that quickly expelled the gastrointestinal nematode pathogen and induced lung inflammation. We’ve now outlined two regulatory effects the nervous system has on the immune response carried out by ILC2s during helminth infection in the gastrointestinal tract: either a dampened one by stimulating the B2-adrenergic receptor or a heightened one by co-localizing cholinergic neurons and ILC2 and activating the NMU receptor 1. A question I still have is, when would the body use one over the other? Why would you want a dampened immune response when infected with a parasite? Is it potentially there to avoid a cytokine storm?
The blog post above mentions that ILC2s express the B2-adrenergic receptor and are found in the intestine close to adrenergic neurons, these neurons release neurotransmitters that interact with the B2-adrengergic receptor and influence the immune response during infection. Ultimately, they found that when mice were infected with a gastrointestinal pathogen and lacked the B2-adrenergic receptor, they had a more exaggerated immune response to the infection in the intestines and lungs which got rid of the parasite quicker. When mice with the B2-adrenergic receptor were infected, they had a weaker immune response which caused the infection to get worse. Thus, they were able to conclude that stimulating the B2-adrenergic receptor on the ILC2s inhibited effector function and cell proliferation. Neural stimulation of the B2-adernergic receptor negatively regulated ILC2-dependent type 2 inflammation. This provides evidence that the nervous system is linked to the immune response via these ILC2s. But the blog post described how it was negatively regulated. I wanted to know if the nervous system was involved in activating ILC2s in orchestrating a strong immune response and if there is another way another way neurons and the nervous system communicated with these ILC2s in the gastrointestinal tract during helminth infection other than via neurotransmitters and the B2-adrenergic receptor. I found this article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6066372/ where they report that ILC2s are the only hematopoietic cells that express the NMU receptor 1 which binds to the neuropeptide neuromedin U (NMU) on cholinergic neurons in the gastrointestinal tract which allows the two cells to co-localize. When the ILC2s were stimulated by NMU in vivo, the cells were rapidly activated, proliferated, and secreted type 2 cytokines IL-5, IL-9, and IL-13. When the cells were administered NMU in vivo, the ILC2s were activated and proliferated and they recruited eosinophils that quickly expelled the gastrointestinal nematode pathogen and induced lung inflammation. We’ve now outlined two regulatory effects the nervous system has on the immune response carried out by ILC2s during helminth infection in the gastrointestinal tract: either a dampened one by stimulating the B2-adrenergic receptor or a heightened one by co-localizing cholinergic neurons and ILC2 and activating the NMU receptor 1. A question I still have is, when would the body use one over the other? Why would you want a dampened immune response when infected with a parasite? Is it potentially there to avoid a cytokine storm?
After reading through the blog post, it was evident how much of an impact innate lymphoid cells have on multiple parts of the body. I was interested to learn more about their function to gain more understanding and see how they work in the immune system. I came across the article entitled “Group 2 Innate Lymphoid Cells (ILC2) Suppress Beneficial Type 1 Immune Responses During Pulmonary Cryptococcosis.” The writers largely discussed a harmful pathogen known as Cryptococcus neoformans that specifically attacks individuals that have received organ transplants as well as other immunocompromised people. ILC2 cells cause a decrease in the type 2 immune system response due to a lack of a transcription factor known as RAR that weakens the function of immune system cells against a harmful agent. For individuals that are immunocompromised, their already weakened immune system makes it even harder to fight off illness. The fungus has been correlated with Pulmonary Cryptococcosis, which is a disease that chronically infects the lungs, as discussed in the post above. The researchers in the study were interested in seeing how ILC2 cells are connected to this infection, and discovered that within mice models there was a significant decrease of ILC2 cells if the mice were infected with the pathogen. Due to the increased number of cells there were less notable cytokines present as well, such IL-4 and IL-5, to combat infection against the pathogen. Cytokines are protein molecules that work specifically in the inflammatory immune response. For the models that had the necessary ILC2 cells, there was proper macrophage function and phagocytosis of Cryptococcus neoformans. To better understand how the immune response works, it is important for us to try and comprehend all components of the immune system to avoid the spread of infection.
Reference : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034304/